| Acute and chronic hepatitis |
Hepatitis

You are called to see a 7-year-old for a well-child visit
Patient
- Gender: Female
- Age: 7 years
- Weight: 47.4 lb./21.5 kg
- Height: 47.9 in/121.7 cm
Vitals
- Blood Pressure: 106/55
- Heart Rate: 82
Signs and Symptoms
Click here to work through this patient case simulation.
Symptoms: Tea-colored urine, vague abdominal discomfort, nausea, pruritus, pale stool
Hepatitis A
Patient will present as → a 38-year-old female who has just returned from a 2-week trip to Mexico. She complains of nausea, vomiting, loss of appetite, and right upper quadrant abdominal pain. She has been sick for the past 3 days. She complains of passing dark-colored urine for the past 2 days. She has had no exposure to blood products, has no history of intravenous drug use, and has no significant risk factors for sexually transmitted disease. On examination, she looks acutely ill. Her pulse is 100 beats/minute, blood pressure 110/70 mm Hg, respirations 18, and temperature 101°F. Her sclerae are icteric, and her liver edge is tender.
- Acute - fatigue malaise, nausea, vomiting, anorexia, fever, and right upper quadrant pain.
- Transmission: Fecal-oral
- DX: Serum IgM anti-HAV
- The IgG antibody to HAV (IgG anti-HAV) test is done to help distinguish acute from prior infection. A positive IgG anti-HAV suggests prior HAV infection or acquired immunity
- TX: Supportive care
- Vaccine: killed (inactivated) - given in two doses
- Routine vaccination beginning at age 1 is recommended for all.
- Vaccinate people at risk (e.g., travelers to endemic areas, laboratory workers), and provide postexposure prophylaxis with standard immune globulin or, for some, vaccination
Hepatitis B
Patient will present as → a 37-year-old male presents to the occupational health clinic after a needlestick exposure in a patient with cirrhosis. In addition to a standard bloodborne pathogen laboratory panel sent for all needlestick exposures at his hospital, additional hepatitis panels are ordered. The patient’s results are shown below:
- HIV 4th generation Ag/Ab: Negative/Negative
- Hepatitis B surface antigen (HBsAg): Negative
- Hepatitis C antibody: Negative
- Anti-hepatitis B surface antibody (HBsAb): Positive
- Anti-hepatitis B core IgM antibody (HBc IgM): Negative
- Anti-hepatitis B core IgG antibody (HBc IgG): Positive
- Acute and Chronic
- Transmission: Sexual or sanguineous
- Serology:
- HBeAg – highly infectious
- HBsAg – ongoing infection
- Anti-HBc – had/have infection
- IgM – acute
- IgG – not acute
- Anti-HBs – immune
- Risk of hepatocellular carcinoma
- Vaccine is given to all infants (birth, 1-2 mo, 6-18 mo)
Hepatitis C
Patient will present as → a 55-year-old rock musician who comes to the office because he has been feeling increasingly tired for 6 months. He has a history of intravenous drug use and alcohol abuse. He states that he feels quite tired but otherwise has no complaints. The examination is non-contributory. His laboratory investigations are normal, aside from elevated liver enzymes.
- Chronic
- Asymptomatic
- Transmission: IV drug use is most common. Also, sexual or sanguineous
- Screen with testing for anti-HCV antibodies
- Diagnosis with HCV RNA quantitation
- Risk of cirrhosis and hepatocellular carcinoma
- Treatment: antiretrovirals target complex of enzymes needed for HCV RNA synthesis
Hepatitis D
- Hepatitis D occurs only when coinfected with Hepatitis B
- Risk of hepatocellular carcinoma
- Suspect hepatitis D particularly when cases of hepatitis B are severe or when symptoms of chronic hepatitis B are worsening
- DX: If serologic tests for hepatitis B confirm infection and clinical manifestations are severe, antibody to HDV (anti-HDV) levels should be measured
- Anti-HDV implies active infection. It may not be detectable until weeks after the acute illness.
- Treat and prevent infection as for hepatitis B.
Hepatitis E
Patient will present as → a 33-year-old Caucasian woman who comes to the emergency department because of vomiting and fever. The patient works as a global health nurse, and her medical history is relevant for recent travel to India. Upon further questioning, the patient mentions that she is concerned because it has been 9 weeks since her last menstruation. Physical examination shows yellowing of the skin and sclera, right upper quadrant tenderness, and hepatomegaly. Her temperature is 101.3°F, pulse is 98/min, respirations are 14/min, and her blood pressure is 120/70 mmHg. Laboratory studies reveal increased aminotransferase levels and a positive pregnancy test.
- Pregnant women, third world countries
- Hepatitis E + mother = high infant mortality
Treatment: Supportive. Vaccinate against other viral hepatitis. HIV treatment PRN.
- Hepatitis C: Direct-acting antiretrovirals target complex of enzymes needed for HCV RNA synthesis
Alcoholic Hepatitis
- Liver enzymes: AST:ALT ratio > 2:1
Toxic Hepatitis
- Acetaminophen toxicity: Treatment with N-Acetylcysteine within 8-10 hrs
Fatty Liver Disease:
Patient will present as → a 43-year-old obese woman with a history of diabetes presents for a routine visit. She denies having any complaints. On physical exam, her physician notices mild hepatomegaly without tenderness to palpation. A liver enzyme panel is sent and reveals elevated transaminases. She is sent for a hepatic ultrasound to evaluate for nonalcoholic fatty liver disease or steatohepatitis.
- Risk factors: Obesity, hyperlipidemia, insulin resistance
- DX: Liver function panel: ALT > AST, elevated alkaline phosphatase, viral hepatitis panel to exclude viral cause of chronic hepatitis
- Ultrasound of liver for all patients - findings steatohepatitis (increased echogenicity and coarsened echotexture of the liver)
- Liver biopsy: large fat droplets (macrovesicular fatty infiltrates)
- TX: lifestyle modification - weight loss, alcohol cessation, diabetes control, low-fat diet
Hepatitis B Serology
| Hepatitis |
Serology |
|
|
|
| Anti-HBc IgM |
Anti-HBc IgG |
HBsAg |
Anti-HBs |
Interpretation |
| + |
- |
+ |
- |
Acute HBV |
| - |
- |
+ |
- |
Early acute HBV |
| - |
+ |
- |
+ |
Resolved acute HBV |
| - |
- |
- |
+ |
HBV vaccine/Immunity |
| - |
- |
- |
- |
No infection or immunity |
| - |
+ |
+ |
- |
Chronic HBV |
Hepatitis C Serology
|
HCV RNA |
Anti-HCV |
| Acute Hepatitis C |
+ |
± |
| Resolved Hepatitis C |
- |
± |
| Chronic Hepatitis C |
+ |
+ |
Hepatitis A Serology
|
IgM HAV Ab |
IgG HAV Ab |
| Acute Hepatitis A |
+ |
|
| Past exposure |
- |
+ |
|
| Acute Liver Failure |
Patient will present as → a 48-year-old female with jaundice, severe fatigue, confusion, increasingly drowsy and disoriented after taking high doses of acetaminophen. Examination shows jaundiced skin and sclerae. Tests reveal markedly elevated liver enzymes, INR 3.2, total bilirubin: 6.5 mg/dL, creatinine: 2.0 mg/dL, and elevated serum ammonia, suggesting acute liver failure from acetaminophen toxicity. The patient is stabilized, given N-acetylcysteine (NAC), and transferred to the ICU. You correct the coagulopathy with FFP and vitamin K, manage cerebral edema with mannitol, and give lactulose to decrease ammonia. You consult a hepatologist and assess for liver transplantation. Acute liver failure is characterized by rapid deterioration of liver function, particularly the synthesis of clotting factors and toxin clearance, in someone without pre-existing liver disease
- The most common cause in the US is acetaminophen overdose
- Common laboratory findings include elevated aminotransferases (AST, ALT), elevated bilirubin, prolonged prothrombin time (PT), and increased INR, low glucose, and elevated ammonia
- Common complications include cerebral edema and intracranial hypertension, coagulopathy and bleeding, renal failure, sepsis, and metabolic derangements
DX: Diagnostic criteria include the presence of coagulopathy (INR ≥ 1.5), the presence of hepatic encephalopathy, the absence of preexisting liver disease, and the duration of illness < 26 weeks
- Acetaminophen level, viral hepatitis serologies, autoimmune markers (ANA, ASMA, IgG), toxicology screen, pregnancy test in women of childbearing age, and abdominal ultrasound or CT scan to rule out chronic liver disease or obstruction
TX: N-acetylcysteine (NAC) is used to treat acetaminophen toxicity but can also benefit other causes by improving hepatic blood flow and oxygen delivery
- Liver transplantation is the definitive treatment for patients with fulminant liver failure who are unlikely to recover with supportive care alone
|
| Cirrhosis (ReelDx) |
Cirrhosis
 You are called to see a 60-year-old with a distended abdomen
You are called to see a 60-year-old with a distended abdomen
Patient
- Gender: male
- Age: 60 years
Vitals
- Temperature: 98.5 F/36.9 C
- Blood Pressure: 156/84
- Heart Rate: 68
- Respiratory Rate: 16
- Pulse Oximetry: 99% RA
Signs and Symptoms
- Distention of abdomen, positional SOB
Click here to work through this patient case simulation.
Patient will present as → a 63-year-old white male with a chief complaint of blood in his stool. He is accompanied by his wife who also reports weight gain, abdominal distension, and swelling of his legs. Physical exam reveals a healthy-appearing male with 3+ bilateral lower extremity edema and distended abdomen with evidence of shifting dullness. You also note several skin lesions seen here. The patient is hemoccult positive and has blood on his urine dipstick. He denies tobacco and illicit drug use but admits to drinking 1-2 x per week and has about 6 beers on each occasion. A chronic liver disease characterized by fibrosis, disruption of the liver architecture, and widespread nodules in the liver
- The most common cause is an alcoholic liver disease
- The second most common cause is chronic hepatitis B and C infections
- Labs: typically AST > ALT
- ↑ risk for hepatocellular carcinoma - 10-25% of patients with cirrhosis - monitor AFP
- Hepatic vein thrombosis (Budd Chiari Syndrome): a triad of abdominal pain, ascites, and hepatomegaly
Distortion of liver anatomy causes
- Portal HTN: decreased blood flow through the liver → hypertension in portal circulation; causes ascites, peripheral edema, splenomegaly, varicosity of veins
- Ascites - accumulation of fluid in the peritoneal cavity due to portal HTN and hypoalbuminemia
- The most common complication of cirrhosis
- Abdominal distension, shifting fluid dullness, fluid wave
- Abdominal ultrasound, diagnostic paracentesis - measure serum albumin gradient
- Salt restriction and diuretics (furosemide and spironolactone)
- Paracentesis if tense ascites, SOB, or early satiety
- Esophageal variceal rupture - dilated submucosal veins, retching or dyspepsia, hypovolemia, hypotension, and tachycardia
- Hepatorenal syndrome: progressive renal failure in ESLD, secondary to renal hypoperfusion from vasoconstriction - azotemia (elevated BUN), oliguria (low urine output, and hypotension
- Hepatic encephalopathy: ammonia accumulates and reaches the brain causing ↓ mental function, confusion, poor concentration
- Asterixis (flapping tremor) - have patient flex hands
- Dysarthria, delirium, and coma
- Hepatocellular failure → decreases albumin synthesis and clotting factor synthesis
- Prolonged PT - PTT in severe disease - treat with fresh frozen plasma
Presentation:
- Ascites, pulmonary edema/effusion, esophageal varices, Terry’s nails (white nail beds)
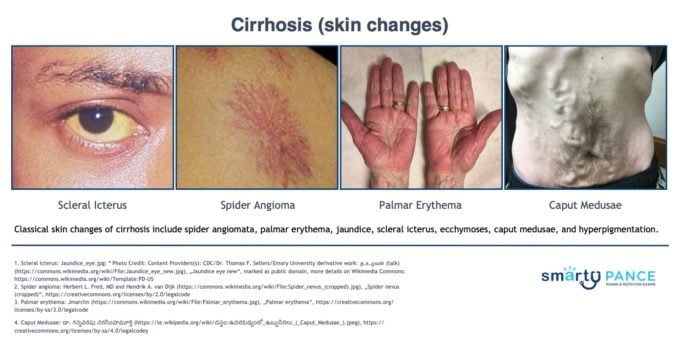
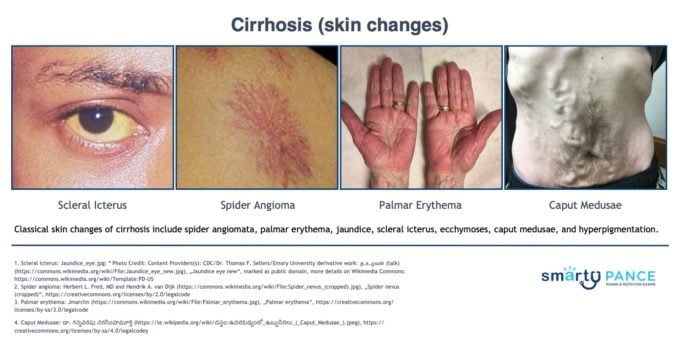
- Skin changes: spider angiomata, palmar erythema, jaundice, scleral icterus, ecchymoses, caput medusae, hyperpigmentation
Treatment: Avoid alcohol, restrict salt, transplant
- Monitoring: periodic lab values q 3 to 4 months (CBC, renal function, electrolytes, LFT, coagulation panel), perform endoscopy for varices, CT-guided biopsy for hepatocellular carcinoma
|
| Nonalcoholic fatty liver disease (NAFLD)
AKA
Metabolic dysfunction-associated steatotic liver disease (MASLD) |
Patient will present as → a 52-year-old female with type 2 diabetes and obesity reporting right upper quadrant discomfort. She does not consume alcohol. Exam shows BMI 33 kg/m² and mild hepatomegaly. Labs reveal elevated ALT (65 U/L) and AST (45 U/L), HbA1c 7.2%. Liver ultrasound shows steatosis. FibroScan® indicates mild fibrosis, suggesting early-stage MASLD (metabolic dysfunction-associated steatotic liver disease), previously termed NAFLD. Treatment focuses on weight loss through diet and exercise. Referral to a dietitian is made. Optimizing glycemic control is advised. Regular follow-ups are scheduled to monitor liver enzymes and aggressively manage diabetes and dyslipidemia. Metabolic dysfunction-associated steatotic liver disease (MASLD), previously termed Nonalcoholic Fatty Liver Disease (NAFLD), is a spectrum of liver conditions NOT related to alcohol consumption
- The spectrum ranges from simple steatosis to nonalcoholic steatohepatitis (NASH)/metabolic dysfunction-associated steatohepatitis (MASH), which can progress to cirrhosis and hepatocellular carcinoma
Patients with MASLD alone have
- Fatty liver (>5 percent hepatic steatosis) with at least one risk factor for cardiometabolic dysfunction, such as dyslipidemia or obesity
- No other causes of steatotic liver disease
- Minimal or no alcohol consumption (i.e., <20 g daily for females and <30 g daily for males)
DX: Diagnosis is often made incidentally when imaging studies (ultrasound, CT, MRI) show fatty liver in the absence of significant alcohol consumption
- Liver function tests may show mild to moderate elevation in ALT and AST, typically with an AST/ALT ratio <1, unlike alcoholic liver disease
- Absence of hepatitis B and C
- The definitive diagnosis can be made with a liver biopsy, showing steatosis, lobular inflammation, and ballooning, but this is NOT routinely performed due to its invasive nature
- Non-invasive markers and scoring systems (e.g., Fibrosis-4 index, NAFLD fibrosis score) can help assess liver fibrosis risk
Monitoring
- ALT every three to six months after patients implement lifestyle interventions to achieve and maintain their weight loss goals
- Noninvasive assessment of fibrosis every three to four years
TX: The mainstay of treatment is lifestyle modification to reduce weight and control metabolic risk factors
MASLD vs. MASH
While MASH is a subset of MASLD, not everyone with fatty liver will develop MASH!
| Feature |
MASLD |
MASH |
| Definition |
Fat buildup in the liver (>5% hepatic steatosis) |
Fat buildup in the liver + inflammation and damage
Patients with MASH have histologic evidence of inflammation + hepatocellular injury, such as ballooning of hepatocytes, with or without fibrosis. |
| Severity |
Generally less severe |
More severe, increased risk of complications |
| Symptoms |
Often none in early stages |
May experience fatigue, abdominal pain, jaundice in later stages |
| Progression |
Can be stable, may progress to NASH |
Can lead to cirrhosis, liver failure, liver cancer |
|