A 22-year-old female with syncope and a head laceration
Patient will present as → a 68-year-old female with a syncopal episode that lasted less than 1 minute. She states she felt nauseous prior to losing consciousness. She has no significant past medical history. Resting blood pressure is 132/84 mm Hg. ECG is normal.
Syncope is a sudden, brief loss of consciousness (LOC) with loss of postural tone followed by spontaneous revival. The patient is motionless and limp and usually has cool extremities, a weak pulse, and shallow breathing. Sometimes brief involuntary muscle jerks occur, resembling a seizure.
Near-syncope is lightheadedness and a sense of an impending faint without LOC. It is usually classified and discussed with syncope because the causes are the same.
Seizures can cause sudden LOC but are not considered syncope. However, seizures must be considered in patients presenting for apparent syncope because history may be unclear or unavailable, and some seizures do not cause tonic-clonic convulsions. Furthermore, a brief (< 5 sec) seizure sometimes occurs with true syncope.
Pathophysiology
Most syncope results from insufficient cerebral blood flow. Some cases involve adequate flow but with insufficient cerebral substrate (O 2 , glucose, or both).
- Insufficient cerebral blood flow
- Most deficiencies in cerebral blood flow result from decreased cardiac output (CO).
- Decreased CO can be caused by
- Cardiac disorders that obstruct outflow
- Cardiac disorders of systolic dysfunction
- Cardiac disorders of diastolic dysfunction
- Arrhythmias (too fast or too slow)
Conditions that decrease venous return
Outflow obstruction can be exacerbated by exercise, vasodilation, and hypovolemia (particularly in aortic stenosis and hypertrophic cardiomyopathy), which may precipitate syncope.
Arrhythmias cause syncope when the heart rate is too fast to allow adequate ventricular filling (eg > 150 to 180 beats/min) or too slow to provide adequate output (eg, < 30 to 35 beats/min).
Venous return can be decreased by hemorrhage, increased intrathoracic pressure, increased vagal tone (which can also decrease heart rate), and loss of sympathetic tone (eg, from drugs, carotid sinus pressure, autonomic dysfunction). Syncope involving these mechanisms (except for hemorrhage) is often termed vasovagal or neurocardiogenic and is common and benign.
Orthostatic hypotension, a common benign cause of syncope, results from failure of normal mechanisms (eg, sinus tachycardia, vasoconstriction, or both) to compensate for the temporary decrease in venous return that occurs with standing (see Orthostatic Hypotension).
Cerebrovascular disorders (eg, strokes, transient ischemic attacks) rarely cause syncope because most of them do not involve the centrencephalic structures that must be affected to produce LOC. However, basilar artery ischemia, due to transient ischemic attack or migraine, may cause syncope. Rarely, patients with severe cervical arthritis or spondylosis develop vertebrobasilar insufficiency with syncope when the head is moved in certain positions.
Insufficient cerebral substrate
The CNS requires O 2 and glucose to function. Even with normal cerebral blood flow, a significant deficit of either will cause LOC. In practice, hypoglycemia is the primary cause because hypoxia rarely develops in a manner causing abrupt LOC (other than in flying or diving incidents). LOC due to hypoglycemia is seldom as abrupt as in syncope or seizures because warning symptoms occur (except in patients taking β-blockers); however, the onset may be unclear to the examiner unless the event was witnessed.
The most common causes are
- Vasovagal (neurocardiogenic)
- Idiopathic
Many cases of syncope never have a firm diagnosis but lead to no apparent harm. A smaller number of cases have a serious cause, usually cardiac.
Red flags - certain findings suggest a more serious etiology
- Syncope during exertion
- Multiple recurrences within a short time
- Heart murmur or other findings suggesting structural heart disease (eg, chest pain)
- Older age
- Significant injury during syncope
- Family history of sudden unexpected death, exertional syncope, or unexplained recurrent syncope or seizures
Key Points:
- Diagnosis depends on a careful history, eyewitness accounts, or fortuitous examination during the event.
- Syncope results from global CNS dysfunction, usually from insufficient cerebral blood flow.
- Most syncope results from benign causes.
- Some less common causes involve cardiac arrhythmia or outflow obstruction and are serious or potentially fatal.
- Vasovagal syncope usually has an apparent trigger, warning symptoms, and a few minutes or longer of post-recovery symptoms.
- Syncope from cardiac arrhythmias typically occurs abruptly and with quick recovery.
- Seizures have a prolonged (eg, hours) recovery period.
- If a benign etiology is not clear, driving and use of machinery should be prohibited until the etiology is determined and treated—the next manifestation of an unrecognized cardiac cause may be fatal
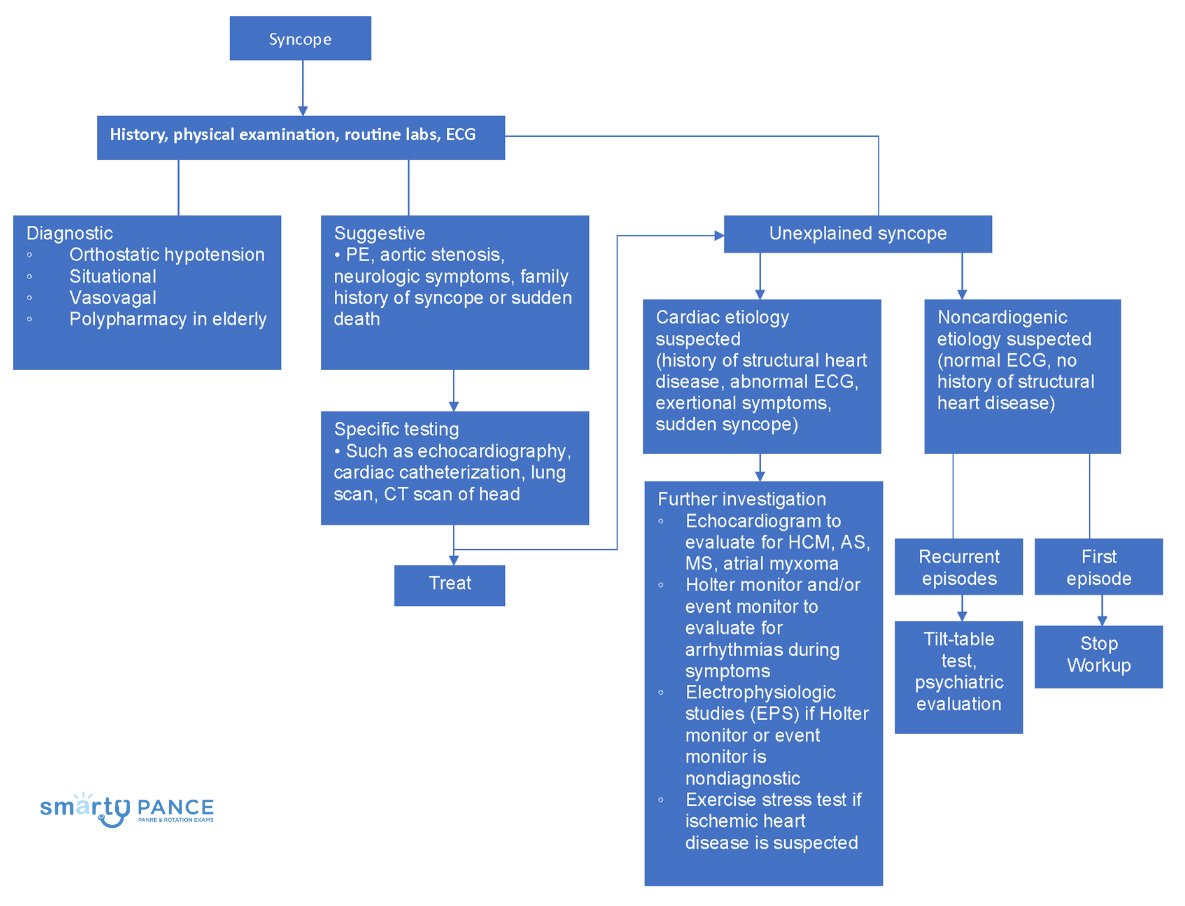
Testing typically includes
- ECG
- Pulse oximetry
- Sometimes echocardiography
- Sometimes, tilt table testing
- Blood tests only if clinically indicated
- CNS imaging rarely indicated
In general, if syncope results in an injury or is recurrent (particularly within a brief period), more intensive evaluation is warranted.
Patients with suspected arrhythmia, myocarditis, or ischemia should be evaluated as inpatients. Others may be evaluated as outpatients.
Treatment is aimed at identifying and fixing the underlying cause
Question 1 |
Loop recorder Hint: Repeating the ECG when she has no symptoms and documented Holter monitor demonstrates the likely etiology of the syncope. | |
Electrophysiology study | |
Exercise treadmill stress test Hint: Exercise treadmill test is not indicated as she has had multiple sustained ventricular tachycardia episodes. | |
Transesophageal echocardiogram Hint: Transesophageal echocardiography is used most commonly to evaluate the aorta for evidence of dissection, to elucidate evidence of atrial clots, and to assess for evidence of valvular vegetations. |
Question 2 |
Vasovagal syndrome | |
AV-nodal re-entrant tachycardia | |
Long QT syndrome | |
Hypertrophic obstructive cardiomyopathy |
Question 3 |
Defibrillation | |
IV adenosine (Adenocard) Hint: Treatment of a hemodynamically stable patient with a tachydysrhythmia is directed at increasing vagal tone either by using vagal maneuvers or drugs. In patients where vagal maneuvers are unsuccessful IV adenosine in increasing doses should be considered. This is followed by the use of either IV calcium channel blockers or IV β-blockers. | |
IV diltiazem (Cardizem) Hint: Treatment of a hemodynamically stable patient with a tachydysrhythmia is directed at increasing vagal tone either by using vagal maneuvers or drugs. In patients where vagal maneuvers are unsuccessful IV adenosine in increasing doses should be considered. This is followed by the use of either IV calcium channel blockers or IV β-blockers. | |
Synchronized cardioversion | |
Vagal maneuvers Hint: Treatment of a hemodynamically stable patient with a tachydysrhythmia is directed at increasing vagal tone either by using vagal maneuvers or drugs. Vagal maneuvers can be accomplished by having the patient bear down, cough, or by unilateral carotid sinus massage. In patients where vagal maneuvers are unsuccessful IV adenosine in increasing doses should be considered. |
|
List |
References: Merck Manual · UpToDate