76 y/o with left leg pain and edema
Patient will present as → a 73-year-old female with complaints of heavy, restless legs and nocturnal cramping of her calves. She has a past medical history of obesity, hypertension, and previous deep venous thromboses after periods of long travel. On physical exam, her bilateral lower legs are edematous with brown hyperpigmentation around the ankles. There are no ulcers. She is scheduled for a duplex ultrasound.
Alternate presentation → a 62-year-old male with a 3.5 mm ulcerated area of the right medial malleolus. The wound is inflamed with associated edema. PMH is significant for varicosities.
Chronic venous insufficiency is impaired venous return, sometimes causing lower extremity discomfort, edema, and skin changes
- Stasis dermatitis is a common skin finding in patients with venous insufficiency
- Severe, nonhealing ulcers commonly at the medial malleolus
- Risk factors: advancing age, family history of venous disease, ligamentous laxity (e.g., hernia, flat feet), prolonged standing, increased BMI, smoking, sedentary lifestyle, lower extremity trauma, prior venous thrombosis (superficial or deep), high estrogen states, and pregnancy
- Postphlebitic (postthrombotic) syndrome is symptomatic chronic venous insufficiency after deep venous thrombosis (DVT).
Diagnosis is based on inspection, but patients should have ultrasonography to rule out DVT
- D-dimer can be used to further clarify the diagnosis and rule out DVT
Treatment is compression, wound care, and rarely surgery
- Leg elevation (when possible) and leg exercises (ankle flexion, walking) to increase calf muscle strength
- Skin changes ("stasis dermatitis") respond to topical dermatologic agents
- Venous ulceration is treated with a combination of ulcer wound management and compression therapy (stockings, bandaging systems).
 Osmosis Osmosis |
|
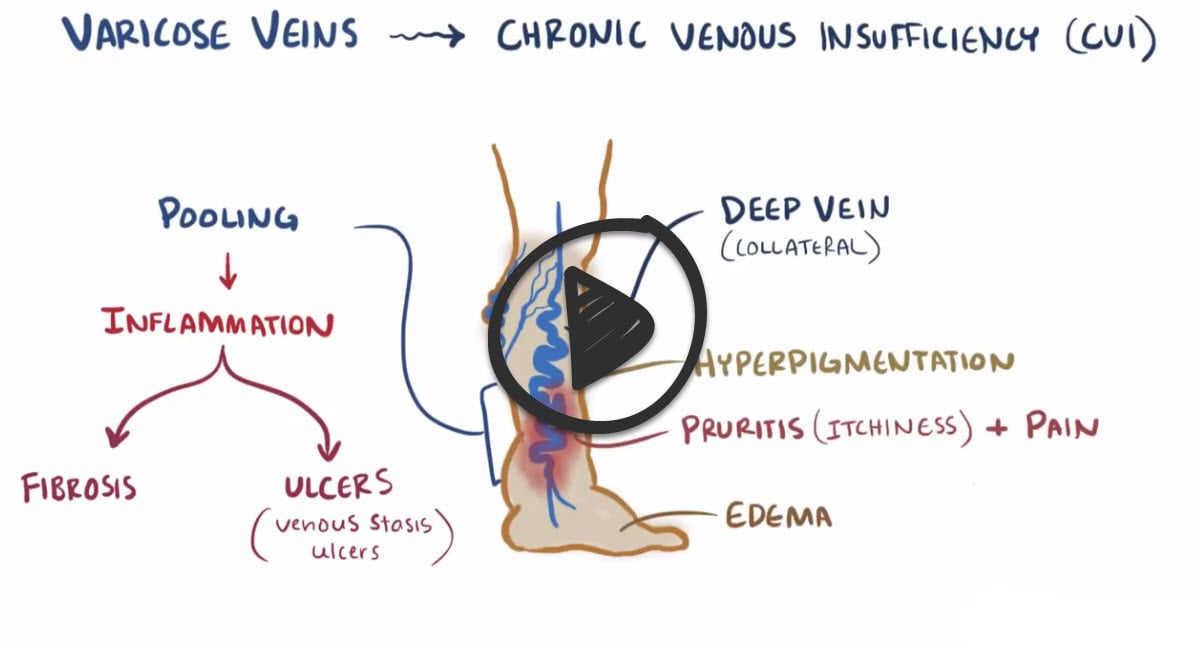 |
Chronic venous insufficiency is a condition that occurs when leg veins and valves fail to maintain blood movement. This can lead to the development of venous stasis ulcers, which are painful and debilitating. With this disorder, patients can have lower leg edema, bronze-brown skin pigmentation, and pruritus. Ulcerations are necrotic with uneven edges and typically occur in the medial malleolus, presenting with dull persistent pain. It is important to note that because the arterial flow is not compromised, the patient’s lower extremities are warm and still have palpable pulses.
Play Video + QuizChronic Venous Insufficiency (Venous Stasis Ulcer) Interventions
Chronic venous insufficiency is a condition that occurs when leg veins and valves fail to maintain blood movement. This can lead to the development of venous stasis ulcers, which are painful and debilitating. In order to promote healing and prevent ulcer recurrence, patients should avoid sitting for long periods of time, use elastic compression stockings, and apply appropriate wound dressings.
Question 1 |
venous insufficiency | |
arterial insufficiency Hint: Patients with arterial insufficiency complain of claudication and they are found to have decreased pulses, distal hair loss, thick nails, and pallor. | |
expected complication of diabetes mellitus Hint: Patients with diabetes that is well controlled may have no symptoms in the lower extremities. | |
peripheral neuropathy Hint: Peripheral neuropathies are not associated with pigmentation changes or edema, although ulcers may develop if the patients have lost their proprioception. |
References: Merck Manual · UpToDate







