Patient with aortic dissection will present as → a 73-year-old female with a history of hypertension, diabetes, and coronary artery disease presents to the emergency department with severe, tearing, knife-like back pain. She states that the pain started approximately 30 minutes ago, and she has felt lightheaded and dizzy ever since its onset. On exam, her vitals are given: T: 98.6 F, HR: 115 bpm, BP: 210/120, RR: 14, SaO2: 97% on room air. CT with contrast is obtained and is demonstrated here.
Patient with an aortic aneurysm will present as → a 72-year-old man with a history of hypertension, coronary artery disease, and smoking who presents for a routine check-up. He mentions no complaints. He has been maintaining his regular activities without any limitations. On examination, the PA notes a subtle, pulsatile enlargement in the patient's abdomen. Given his risk factors, an abdominal ultrasound is performed, which reveals a 5.5 cm infrarenal abdominal aortic aneurysm without evidence of rupture. The patient is asymptomatic but is referred to a vascular surgeon for further evaluation and management.
Abdominal Aortic Aneurism (AAA) = back and flank pain, pulsatile mass, and hypotension
Aortic Dissection = severe, tearing (ripping, knife-like) chest pain radiating to the back
Abdominal Aortic Aneurysm
Abnormal dilation of the aorta caused by a weakening of the arterial wall
Presentation: Flank pain, hypotension, pulsatile abdominal mass
- Screening: Ultrasound, if male > 65 and ever a smoker
- Surgical repair if ≥ 5.5 cm in men or ≥ 5.0 cm in women
- Monitoring and surveillance (see treatment tab)
- Beta-blocker
- The classic presentation is an older male (>60y) with severe back or abdominal pain who presents with syncope and hypotension with a tender pulsatile abdominal mass.
- Unlike dissection, an AAA involves all 3 layers and can be present at various locations
- Males are eight times as likely to have an aortic aneurysm
- > 3.0 cm is usually considered aneurysmal
- Diagnosed by ultrasound CT scan test of choice for further evolution
- Treatment is based on size - see "treatment" section
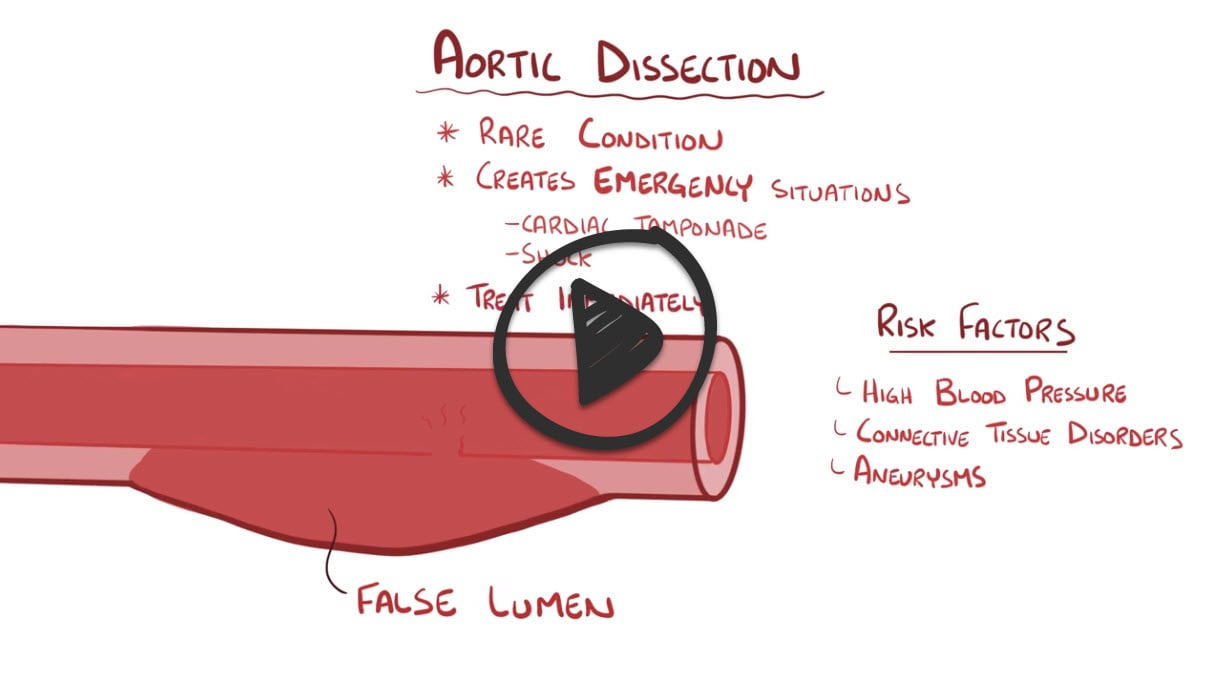
Aortic Dissection
An aortic dissection is a serious condition in which a tear occurs in the inner layer of the body's main artery (aorta)
Presentation: Sudden onset tearing chest pain between the scapula, diminished pulses
- Chest radiograph: Widened mediastinum
- Ascending aorta- Surgical emergency
- Descending aorta- Medical therapy (beta-blockers) unless complications are present
- Aortic Dissection is caused by hypertension and involves only one layer of the arterial lining (the intima)
- Patients will present with SEVERE, TEARING (RIPPING, KNIFE-LIKE) sensation radiating to the back
- Variation in pulse between the right and the left arm
- CT scan is sensitive, can be performed quickly, and allows for rapid intervention.
- MRI angiography is the gold standard for evaluation (in hemodynamically stable patients)
- Treatment
- Lower Blood pressure
- Type A (Proximal Aortic Dissection)
- Surgical management
- Type B (Distal Aortic Dissection)
- Medical management initially, surgery only if needed
AAA - ultrasound is the initial imaging study of choice, and CT scan is the test of choice for thoracic aneurysms and for further evaluation of patients with known AAA
- Angiography is the GOLD STANDARD for the evaluation of AAA
- Screening: The USPSTF recommends one-time screening for abdominal aortic aneurysm by ultrasonography in men ages 65 to 75 years who have ever smoked
- Evidence is insufficient to recommend this screening in women

Abdominal ultrasonography of a 78-year-old woman in the sagittal plane, showing an abdominal aortic aneurysm, with axial plane diameter annotated by the red dashed line and maximal diameter in the sagittal plane in dotted yellow.
Aortic Dissection:
- CT scan is sensitive for the diagnosis of aortic dissection, can be performed quickly, and allows for rapid intervention. It is the most appropriate first-line diagnostic modality.
- MRI angiography is the gold standard for evaluation
- Chest radiograph: widened mediastinum
Patients with an incidentally discovered AAA < 3 cm in diameter require no further follow-up in the near term
- If initial US screening identified an aortic diameter less than 3 cm but greater than 2.5 cm, rescreening after 10 years is suggested
Repeat Ultrasound
- Every 3 years in all patients with AAA diameter 3.0-3.9 cm
- Annually, in men with AAA diameter of 4.0-4.9 cm or women with AAA diameter of 4.0-4.4 cm
- Every 6 months in men with AAA diameter ≥ 5.0 cm or women with AAA diameter ≥ 4.5 cm
Repair is recommended in men with AAA diameter ≥ 5.5 cm or women with AAA diameter ≥ 5.0 cm and in the setting of symptoms attributable to the aneurysm
Additional indications for elective surgery include
- Increase in aneurysm size by > 0.5 cm within 6 months, regardless of size
- Chronic abdominal pain
- Thromboembolic complications
- Iliac or femoral artery aneurysm that causes lower-limb ischemia
- Aneurysms > 4.5 cm in patients with Marfan syndrome
| AAA Diameter (cm) | Management Recommendation |
|---|---|
| < 3 | No further follow-up is required in the near term |
| 2.5 - < 3 | Rescreen with Ultrasound after 10 years |
| 3.0 - 3.9 | Repeat Ultrasound every 3 years |
| Men: 4.0 - 4.9
Women: 4.0 - 4.4 |
Repeat Ultrasound annually |
| Men: ≥ 5.0
Women: ≥ 4.5 |
Repeat Ultrasound every 6 months |
| Men: ≥ 5.5
Women: ≥ 5.0 |
Repair is recommended |
| Additional Indications for Surgery | Increase in aneurysm size by > 0.5 cm within 6 months
Chronic abdominal pain Thromboembolic complications Iliac or femoral artery aneurysm causing lower-limb ischemia Aneurysms > 4.5 cm in patients with Marfan syndrome |
-------------------
Management of Dissection
- Lower blood pressure - IV beta-blockers (metoprolol, labetalol, esmolol) to lower HR and diminish the force of LV ejection
- Type A (Proximal Aortic Dissection)
- Surgical management
- Type B (Distal Aortic Dissection)
- Medical management initially, surgery only if needed
 Osmosis Osmosis |
|
 |
|
 |
Abdominal aortic aneurysms are described as dilatations or outpouchings of the endothelial walls of the descending aorta. Rupture of these aneurysms are life-threatening, and patients who have ever smoked between the ages of 65 and 70 should be screened. The diagnostic treatment of choice is ultrasound, and treatment recommendations are as follows: aneurysms that are less than 5 centimeters and asymptomatic should be observed; aneurysms greater than 5.5 centimeters should be surgically repaired; ruptured or symptomatic aneurysms require emergent intervention.
Play Video + QuizAortic Dissection
Aortic dissection is a potentially catastrophic condition initiated by a tear in the aortic intima. There are 2 systems used to classify aortic dissections: Stanford and DeBakey. Under the Stanford classification, type A dissections occur in the ascending aorta while type B dissections are all others. Risk factors include hypertension, aortic aneurysm, and connective tissue disorders like Marfan syndrome. Clinical features of this disease include sudden, severe chest pain that may radiate to the back, blood pressure difference between upper extremities, and mediastinal widening on chest X-ray. Treatment includes surgery for Type A as they carry a risk of dissecting proximally into the pericardium and heart valves. Type B dissections are managed with beta blockers to reduce blood pressure.
Play Video + QuizQuestion 1 |
Aortic dissection | |
Acute myocardial infarction Hint: While AMI can present with severe chest pain, it is typically described as pressure or tightness and may not have the ripping or tearing quality. Additionally, AMI does not usually cause a blood pressure variation between arms or a diastolic murmur. | |
Cardiac tamponade Hint: This condition can cause shock and impaired sensorium due to decreased cardiac output. However, the classic presentation includes Beck's triad (hypotension, muffled heart sounds, and jugular venous distension), not the interscapular pain or blood pressure variation seen in aortic dissection. | |
Pulmonary embolism Hint: PE can present with sudden onset of chest pain, shortness of breath, and signs of shock. However, the pain is more often pleuritic, and PE does not cause a diastolic murmur or blood pressure variation between arms. | |
Thoracic aortic aneurysm Hint: While a thoracic aortic aneurysm may present with chest or back pain, it typically does not cause the acute, severe, ripping or tearing pain associated with dissection. Additionally, aneurysms without dissection are less likely to present with the acute shocky appearance, impaired sensorium, and blood pressure variations indicative of an aortic dissection. |
Question 2 |
Squeezing Hint: This type of pain is more commonly associated with myocardial ischemia or infarction, where the heart muscle does not receive enough blood flow, often described as a pressure or squeezing pain in the chest. | |
Dull, aching Hint: Dull, aching pain is more characteristic of chest wall pain, possibly angina, or anxiety. | |
Ripping, tearing | |
Burning Hint: Burning chest pain is often related to gastroesophageal reflux disease (GERD) or esophageal disorders, rather than cardiovascular conditions like aortic dissection. | |
Sharp and stabbing Hint: While sharp and stabbing pain can occur in various conditions, including pneumothorax or pleuritic pain, it does not capture the distinctive ripping or tearing sensation that is characteristic of aortic dissection. |
Question 3 |
Immediate open surgical repair Hint: An option, but EVAR is preferred for suitable candidates due to its less invasive nature. | |
Endovascular aneurysm repair (EVAR) | |
Serial ultrasound monitoring every 6 months Hint: Recommended for smaller aneurysms (less than 5.5 cm in diameter). | |
Aggressive control of hypertension with medication Hint: Important for overall management but not sufficient alone for an aneurysm of this size. | |
Lifestyle modifications only Hint: Beneficial for cardiovascular health but insufficient for managing a large aneurysm.
|
|
List |
References: Merck Manual · UpToDate





