|
The most common causes include:
Other causes: bronchiectasis, pulmonary catheters, trauma, pulmonary hemorrhage |
|
Small Cell (15% of cases) (central mass) - 99% smokers, does not respond to surgery and metastases at presentation
- Location: Central, very aggressive
- Treatment: Combination chemotherapy needed
- Paraneoplastic syndromes: Cushing's, SIADH
Non-Small Cell (85 percent of lung cancer cases)
- Squamous cell (central mass) with hemoptysis, 25-35% of lung cancer cases
- Location: central
- May cause hemoptysis
- Paraneoplastic syndrome: hypercalcemia
- Elevated PTHrp
- Large cell - fast doubling rates - responds to surgery rare (only 5%)
- Location: Periphery 60%
- Paraneoplastic syndrome: Gynecomastia
- Adenocarcinoma - most common (peripheral mass), 35-40% of cases of lung cancer
- Most common
- Associated with smoking and asbestos exposure
- Location: Periphery
- Paraneoplastic syndrome: Thrombophlebitis
Treatment:
Non-Small Cell can be treated with surgery
- Treatment depends on staging:
- Stage 1-2 surgery
- Stage 3 Chemo then surgery
- Stage 4 palliative
Small Cell: CAN NOT be treated with surgery will need chemotherapy
Associated manifestations:
- Superior vena cava syndrome (facial/arm edema and swollen chest wall veins)
- Pancoast tumor (shoulder pain, Horner’s syndrome, brachial plexus compression)
- Horner’s syndrome (unilateral miosis, ptosis, and anhidrosis)
- Carcinoid syndrome (flushing, diarrhea, and telangiectasia)
|
|
Dyspnea, and a vague discomfort or sharp pain that worsens during inspiration
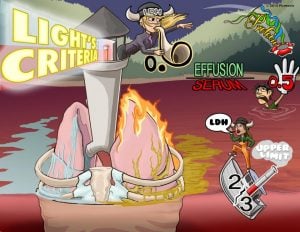
- Differentiate exudate and transudate with pleurocentesis and Light’s Criteria
- Exudate: (local pleural disease) - protein ratio ↑, LDH ↑, infection, malignancy, trauma
- Transudate: Congestive heart failure, atelectasis, cirrhosis
- Decreased tactile fremitus, dullness to percussion, and diminished breath sounds over the effusion
- Lateral decubitus x-ray and upright films: Blunting of the costophrenic angle. A mediastinal shift away from effusion
- Thoracentesis is the gold standard
Picmonic Light’s Criteria
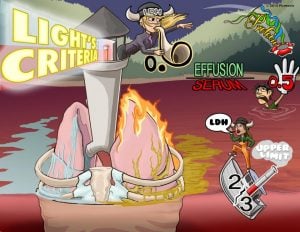 Light’s Criteria is a diagnostic tool used to determine of the cause of a pulmonary effusion; transudate versus exudate. This relies on a comparison of the chemistries in the pleural fluid to those in the blood. According to Light’s criteria, a pleural effusion is likely exudative if at least one of the following exists: The ratio of pleural fluid protein to serum protein is greater than 0.5, the ratio of pleural fluid LDH and serum LDH is greater than 0.6, or the pleural fluid LDH is greater than 0.6 or 2⁄3 times the normal upper limit for serum. Light’s Criteria is a diagnostic tool used to determine of the cause of a pulmonary effusion; transudate versus exudate. This relies on a comparison of the chemistries in the pleural fluid to those in the blood. According to Light’s criteria, a pleural effusion is likely exudative if at least one of the following exists: The ratio of pleural fluid protein to serum protein is greater than 0.5, the ratio of pleural fluid LDH and serum LDH is greater than 0.6, or the pleural fluid LDH is greater than 0.6 or 2⁄3 times the normal upper limit for serum.
Play Video + Quiz
|
|
Currently, postoperative pneumonia is the third most common complication for all surgical procedures and is associated with increased patient morbidity and mortality
- Prolongs the length of stay by a mean of 7 - 9 days as well as increases medical costs ranging from $12,000 to $40,000
- Hospital-acquired pneumonia (pneumonia developing 48 - 72 h after admission)
- Ventilator-associated pneumonia (VAP, pneumonia developing 48 - 72 h after endotracheal intubation) occurring in the post-surgical patient
The most important pathogens are
- Pseudomonas aeruginosa
- Methicillin-sensitive Staphylococcus aureus
- Methicillin-resistant S. aureus (MRSA)
Diagnosis:
- Chest x-ray or chest computed tomography
- Sometimes bronchoscopy or blood cultures
Treatment includes empirically chosen antibiotics active against resistant organisms
- Piperacillin/tazobactam
- Cefepime
- Levofloxacin
- Imipenem
- Meropenem
In treatment settings where MRSA rates are > 20%, vancomycin or linezolid should be added |
|
An absence of breath sounds and hyperresonance to percussion with tracheal deviation
Spontaneous:
- Primary spontaneous pneumothorax occurs in the absence of underlying disease - tall, thin males between 10 and 30 years of age are at the greatest risk of primary pneumothorax
- Secondary spontaneous pneumothorax occurs in the presence of underlying disease - asthma, COPD, cystic fibrosis, interstitial lung disease
Tension:
- Etiology: Penetrating injury
- Physical exam: Hyperresonance to percussion and tracheal shift to the contralateral side
Small pneumothoraces <15% of the diameter of the hemithorax will resolve spontaneously without the need for chest tube placement
- For large, > 15% of the diameter of hemithorax, and symptomatic pneumothoraces, chest tube placement is performed
- Patients should be followed with serial CXR every 24 hours until resolved
|
|
Shortness of breath can have causes that aren't due to underlying disease. Examples include exercise, altitude, tight clothing, a prolonged period of bed rest, or a sedentary lifestyle
- Asthma: SOB, flare-ups, wheezing
- COPD: SOB, fatigue, dry cough
- Pneumonia: SOB, fever, coughing
- Congestive heart failure: SOB, water retention, weight gain
- Acid reflux: SOB, nausea, epigastric pain
- Pneumothorax: tachypnea, shallow breath, SOB
- Pulmonary embolism: SOB, tachycardia, tachypnea, chest pain
- Foreign body aspiration: SOB, inspiratory stridor (if high in the airway), wheezing, and decreased breath sounds if low in the airway
- Interstitial lung disease: SOB, tachypnea, weight loss, chronic cough, fatigue
- Obesity: SOB in the supine position, sleep apnea, weight gain, fatigue, snoring
- Pulmonary hypertension: SOB, fatigue, edema, cough, dizziness, hypotension
- Sarcoidosis: fatigue, eye redness, skin rash, swollen lymph nodes, hilar lymphadenopathy
- Tuberculosis: SOB, hemoptysis, fatigue, fever, weight loss, night sweats
- Anemia: SOB, pallor, brittle nails, tachycardia, lightheadedness, fatigue
- Cardiomyopathy: SOB, fatigue, edema, weight gain
- Pericarditis: SOB, fever, chest pain
- Epiglottitis: dysphagia, drooling, respiratory distress
- Generalized anxiety disorder: fatigue, SOB, irritability, fear, emotional distress, palpitations
- Myasthenia gravis: ptosis, weak chewing, easily fatigued, SOB, weakness in everyday activity (brushing hair)
- Fractured Rib: SOB, chest pain, trauma
- Sudden blood loss
|
|
Weight loss and fatigue can have causes that aren't due to underlying disease. Examples include dieting, exercise, malnutrition, or lack of access to food, lack of sleep, heavy exertion, jetlag, a large meal, or aging
- Chronic obstructive pulmonary disease: fatigue, shortness of breath, dry cough
- Chronic fatigue syndrome: fatigue, anxiety, muscle pain
- Sarcoidosis: fatigue, eye redness, skin rash, swollen lymph nodes, hilar lymphadenopathy
- Interstitial lung disease: SOB, tachypnea, weight loss, chronic cough, fatigue
- Pulmonary hypertension: fatigue, inability to exercise, edema
- Tuberculosis: SOB, hemoptysis, fatigue, fever, weight loss, night sweats
- HIV: fatigue, fever, weight loss, night sweats, opportunistic infections
- Sleep apnea: fatigue, episodes of apnea, weight gain, snoring
- Rheumatoid arthritis: weight loss, fatigue, joint pain
- Hyperthyroidism: weight loss, fatigue, excessive sweating
- Type 1 diabetes: weight loss, fatigue, hunger
- Type 2 diabetes: weight loss, fatigue, excess thirst, excessive hunger
- Clinical depression/Seasonal affective disorder: fatigue, agitation, anxiety
- Anorexia: weight loss, irregular menstruation, underweight
- Insomnia: fatigue, sleeping difficulty, daytime sleepiness
- Anemia: SOB, pallor, brittle nails, tachycardia, lightheadedness, fatigue
- Anxiety disorder: fatigue, anxiety, excessive worry
|