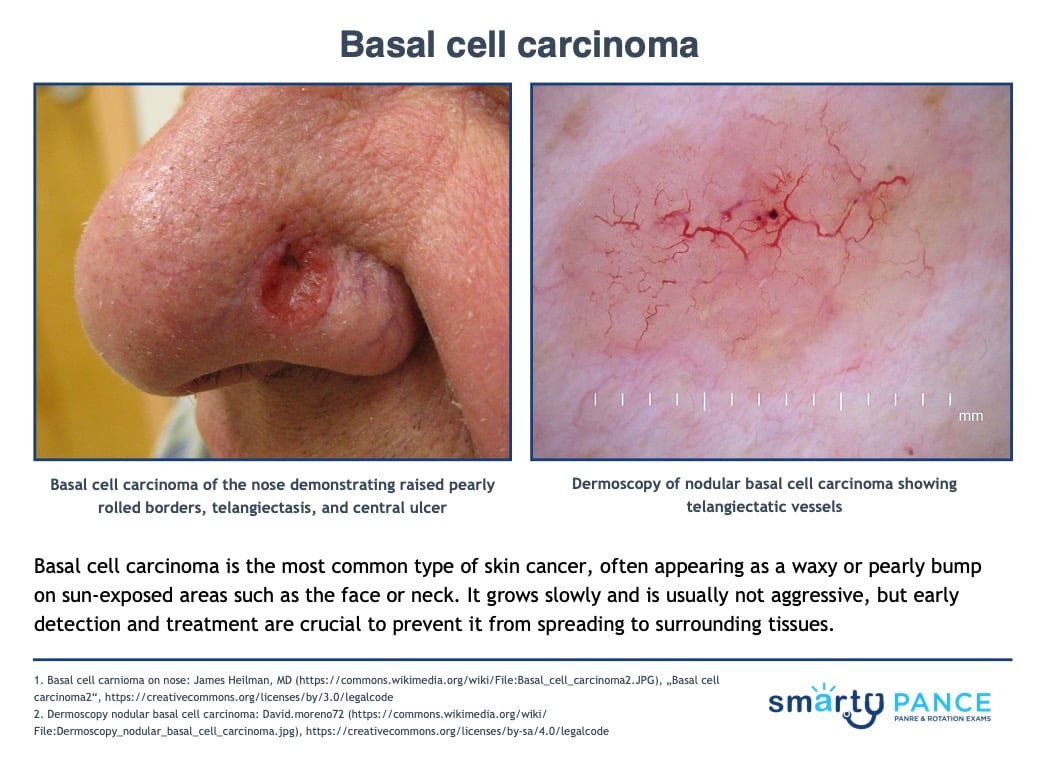
| Basal cell carcinoma |
A type of cancer that begins in the basal cells
- Basal cells produce new skin cells as old ones die. Limiting sun exposure can help prevent these cells from becoming cancerous
- Typically appears as a white waxy lump or a brown scaly patch, raised pearly and rolled borders, telangiectasis, a central ulcer on sun-exposed areas, such as the face and neck
DX: All lesions suspicious for basal cell carcinoma should undergo either a shave or punch biopsy prior to initiating curative treatment
TX: Treatments include prescription creams fluorouracil (FU) and imiquimod, photodynamic therapy (PDT), and surgical excision with clear margins
|
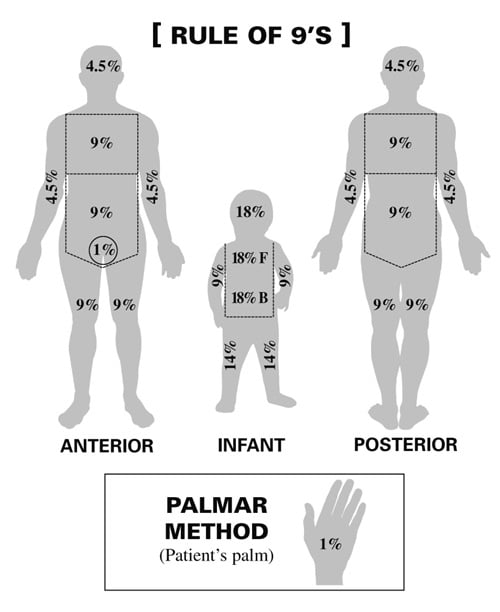
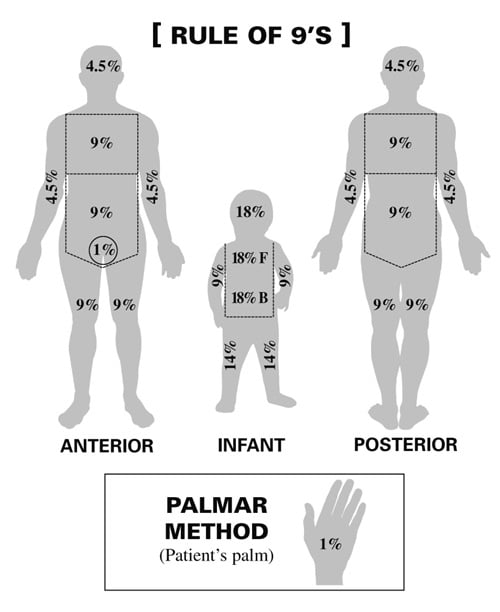
| Burns |
Body percentage:
- Rule of 9’s: Head 9%, Each arm 9%, Chest 9%, Abdomen 9%, Each anterior leg 9%, Each posterior leg 9%, Upper back 9%, Lower back 9%, Genitals 1%
- Palmar method: Patient’s palm equates to 1%
Degree involvement:
Treatment: Monitor ABCs, fluid replacement, and sulfadiazine. Children with > 10% total body surface area and adults with > 15% total body surface area burns need formal fluid resuscitation
|
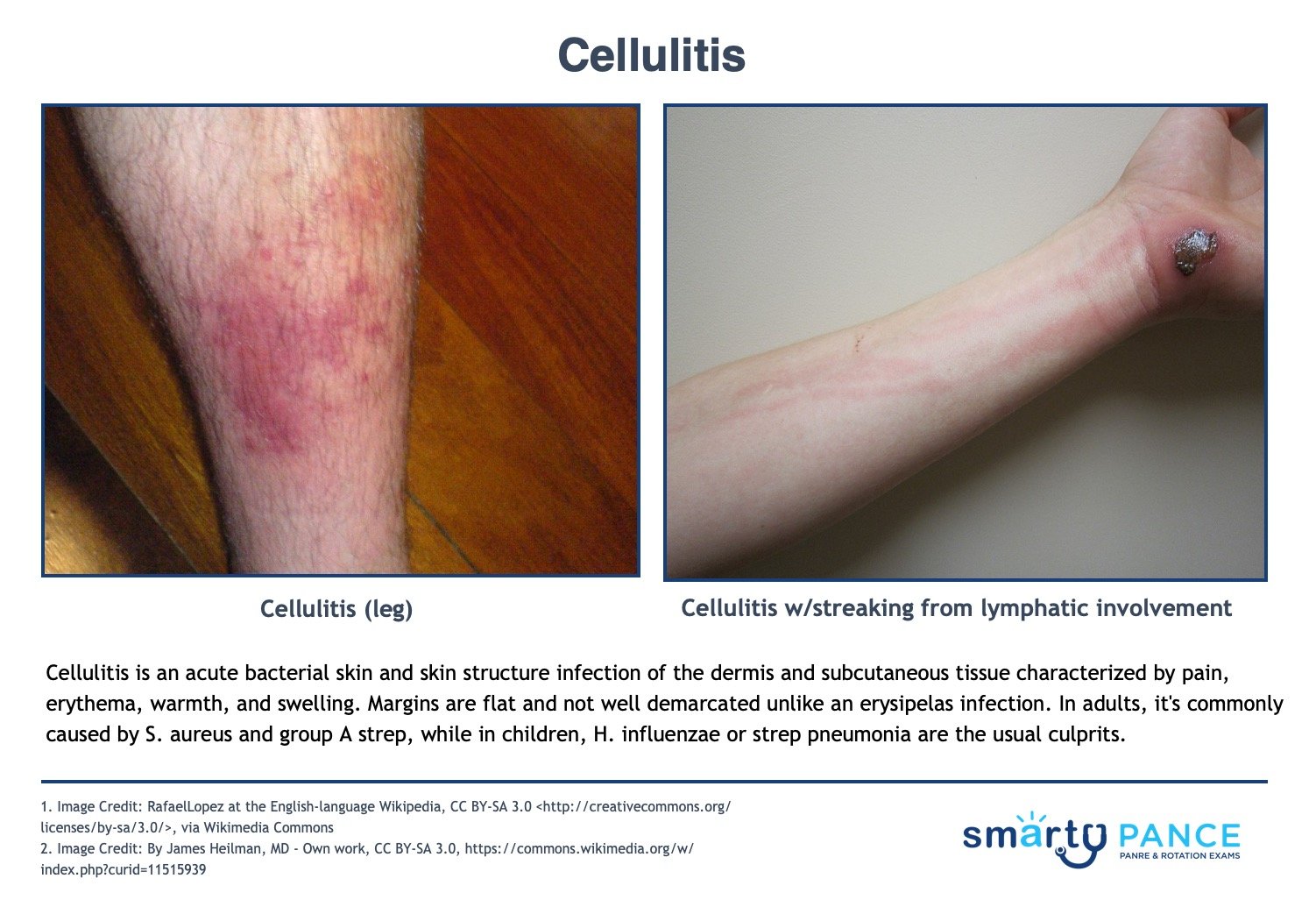
| Cellulitis |
An acute bacterial skin and skin structure infection of the dermis and subcutaneous tissue characterized by pain, erythema, warmth, and swelling. Margins are flat and not well demarcated.
- Caused by Staphylococcus and Streptococcus in adults
- H. influenzae or strep pneumonia in children
- Cellulitis does not have sharp, well-defined borders, unlike an erysipelas infection
DX: Culture should be taken of all purulent wounds and followed up in 48 hours
Treat mild cellulitis (MSSA)
- Cephalexin 500 mg QID x 5-7 days
- Cefuroxime 500 mg BID x 5-7 days
- If PCN allergy - Clindamycin 450 mg TID x 5-7 days
Cat bites with augmentin or doxycycline if PCN allergic
Puncture wound with Cipro (cover pseudomonas)
Treat purulent or methicillin-resistant Staphylococcus aureus infection (MRSA) with
- Trimethoprim-sulfamethoxazole (TMP-SMZ) 1 DS tab PO BID x 7 days
- Clindamycin 450 mg PO TID x 7 days
- Doxycycline 100 mg PO BID x 8 days
- Intravenous Vancomycin or Linezolid
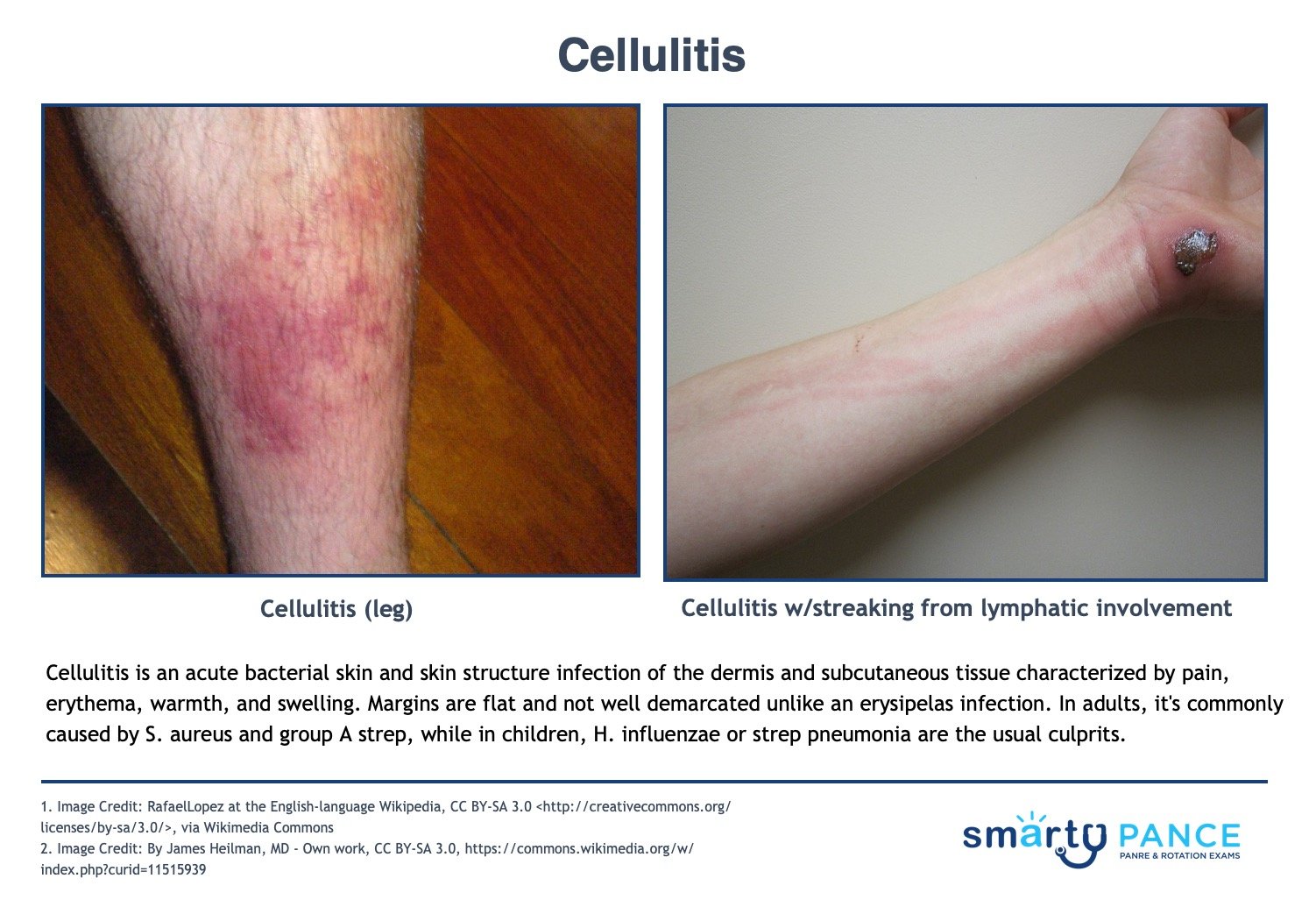
View more images of cellulitis |
| Discharge |
Breast/nipple discharge
- Mastitis/Breast abscess: nipple discharge, redness, warm skin
- Breast Cancer: nipple discharge, breast discomfort, breast mass
- Gynecomastia: nipple discharge, breast enlargement, overweight
- Inflammatory breast cancer: nipple discharge, breast enlargement, redness
- Hypogonadism: nipple discharge, sexual dysfunction, reduced sex drive
GU
- Infections of the vagina, such as a yeast infection, bacterial vaginosis, trichomoniasis, human papillomavirus (HPV), or herpes
- Infection of the cervix (cervicitis)
- An object in the vagina, such as a forgotten tampon
- Sexually transmitted infections (STIs), such as chlamydia or gonorrhea
- Various sex practices, such as oral-to-vaginal and anal-to-vaginal contact
- Vaginal medicines or douching
- Menopause: vaginal discharge, an absence of menstruation, anxiety
Other skin conditions
- Abscess: pain, redness, with or without discharge
|
| Drug eruptions (postoperative) |
Drug-induced exanthems are the most common cutaneous reactions to drugs, responsible for approximately 90 percent of all drug rashes
- The most commonly prescribed medications (eg, antibiotics, sulfonamides) are implicated in most cases
Clinical evaluation and skin biopsy - shows necrotic epithelium
- Diagnosis is often obvious from the appearance of lesions and rapid progression of symptoms. Histologic examination of sloughed skin shows necrotic epithelium, a distinguishing feature.
- Differential diagnosis in SJS and early TEN include erythema multiforme, viral exanthems, and other drug rashes
Stop all potentially offending medications
- Early admission to burn unit or pediatric intensive care unit for initial stabilization and management of fluid, electrolytes, and nutrition; airway stability; and eye care
- Prompt ophthalmology and dermatology consultation
- Intravenous immunoglobulin (IVIG)
- Steroids used to be the treatment of choice are now thought to be an increased risk for sepsis
|
| Melanoma |
Usually a pigmented lesion with an irregular border, irregular surface, or irregular coloration
Melanoma occurs when the pigment-producing cells that give color to the skin (melanocytes) become cancerous
- Symptoms might include a new, unusual growth or a change in an existing mole. Melanomas can occur anywhere on the body
- Asymmetrical, unevenly pigmented patch/plaque with a nodule and an irregular border
ABCDE: A symmetry, B order is irregular, C olor variability (blue, red, white), D iameter (increasing or > 6 mm), E volving (changing in size, shape, or color)
DX: Diagnosis is by biopsy - If doubt exists, biopsy should include the full depth of the dermis and extend slightly beyond the edges of the lesion
Prognosis of melanoma is most strongly associated with the depth of the lesion, based on the Clark Classification System of Microstaging
- Clark Classification System of Microstaging
- Level I: Confined to the epidermis (in situ)
- Level II: Invasion into the papillary dermis
- Level III: Penetration to the papillary-reticular interface
- Level IV: Invasion into the reticular dermis
- Level V: Penetration into the subcutaneous fat
TX: Treatment may involve Mohs surgery, radiation, medications, or in some cases chemotherapy

View more images of melanoma |
| Pressure ulcers |
The sacrum and hip are most often affected. Reposition every 2 hours
- Stage 1: erythema of localized area, usually non-blanching over the bony surface
- Stage 2: partial loss of dermal layer, resulting in pink ulceration
- Stage 3: full dermal loss, often exposing subcutaneous tissue and fat
- Stage 4: full-thickness ulceration exposing bone, tendon, or muscle. Osteomyelitis may be present
Wound management by stage of the ulcer
- Stage I: aggressive preventive measures, thin-film dressings for protection
- Stage II: occlusive dressing to maintain healing, transparent films, hydrocolloids
- Stages III-IV: Débridement of necrotic tissue. Exudative ulcers will benefit from absorptive dressings such as calcium alginates, foams, and hydrofibers. Dry ulcers require occlusive dressing to maintain moisture, including hydrocolloids, and hydrogels.
Risk factors: age >65, impaired circulation, immobilization, undernutrition, incontinence
DX: based on observation and staged according to classification
TX: debridement ⇒ depends on the extent of necrosis; surgical closure may be necessary; vacuum-assisted closure uses negative pressure to reduce wound edema and remove debris/reduce bacterial load
 Image: YOLO-Based Deep Learning Model for Pressure Ulcer Detection and Classification - Scientific Figure on ResearchGate by CC 4.0 |
| Rash |
Rashes in the context of general surgery are a common yet often overlooked complication. These rashes can arise from various causes, ranging from allergic reactions to infections, and their management is crucial for patient recovery and comfort.
Causes of Surgical Rashes
- Incisional Rashes: These occur around surgical incisions and may be due to irritation from sutures, dressings, or the healing process itself.
- Drug-Related Rashes: Commonly caused by reactions to medications administered during or after surgery, such as antibiotics or anesthesia.
- Infectious Rashes: These include cellulitis or surgical site infections, often characterized by redness, swelling, and warmth.
- Allergic Reactions: These can be due to latex, adhesives, or other materials used in the surgical setting.
Diagnosis and Assessment
Diagnosing a surgical rash involves a thorough patient history and physical examination. Key diagnostic tools may include:
- Skin Biopsy: To examine the tissue under a microscope.
- Culture Tests: To identify any infectious agents.
- Blood Tests: To check for systemic signs of infection or allergic reaction.
Management and Treatment
The treatment of surgical rashes depends on the underlying cause:
- For Incisional Rashes:
- Gentle cleaning and appropriate wound care.
- Monitoring for signs of infection.
- For Drug-Related Rashes:
- Discontinuing the offending drug.
- Administration of antihistamines or steroids in case of severe reactions.
- For Infectious Rashes:
- Antibiotics for bacterial infections.
- Proper wound care and hygiene.
- For Allergic Reactions:
- Identification and avoidance of the allergen.
- Use of antihistamines or corticosteroids to reduce symptoms.
Prevention
Preventive measures are key in the surgical setting. These include:
- Using hypoallergenic materials for sutures and dressings.
- Careful selection and monitoring of drugs used during and after surgery.
- Maintaining strict aseptic techniques to prevent infections.
|
| Redness/erythema |
In the realm of general surgery, redness or erythema around a surgical site is a common observation. It's crucial for healthcare professionals, especially those in surgical care, to understand the implications of erythema and how to manage it effectively.
What is Erythema?
Erythema refers to redness of the skin, often a sign of irritation, inflammation, or infection. In a post-surgical context, it can be a normal part of the healing process, but it may also indicate complications such as infection or an allergic reaction.
Causes of Erythema in Surgery
- Normal Healing Response: Mild erythema can be part of the body's natural healing process post-surgery.
- Infection: More pronounced or spreading redness, especially when accompanied by warmth, pain, or discharge, can signal an infection.
- Allergic Reaction: Redness could be a reaction to sutures, dressings, or other materials used in surgery.
- Inflammation: Due to tissue trauma during surgery.
Diagnosis and Assessment
To diagnose the cause of erythema, consider:
- Duration and Spread: How long has the redness been present, and is it spreading?
- Associated Symptoms: Look for pain, swelling, heat, or discharge.
- Patient History: Consider any allergies or previous reactions to surgical materials.
Management and Treatment
The approach to managing erythema depends on its cause:
- For Normal Healing:
- Monitor the area for changes.
- Educate the patient on what to watch for in terms of worsening symptoms.
- For Infection:
- Administer appropriate antibiotics.
- Provide wound care and possibly drainage if needed.
- For Allergic Reactions:
- Identify and remove the allergen.
- Treat with antihistamines or corticosteroids as needed.
- For Inflammation:
- Use of anti-inflammatory medications.
- Ensure proper wound care and rest.
- Prevention
Preventive strategies include:
-
- Using hypoallergenic materials.
- Adhering to sterile techniques to reduce infection risk.
- Preoperative assessments for any known allergies or sensitivities.
|
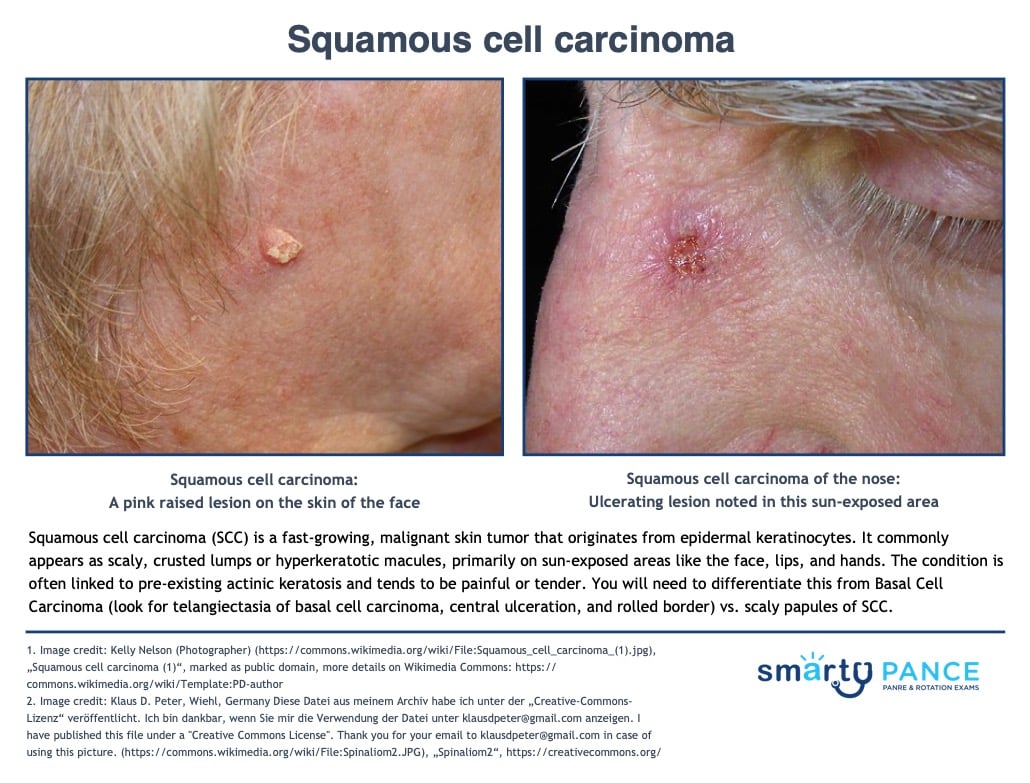
| Squamous cell carcinoma |
Raised, slightly pigmented skin lesion; ulceration/exudate; chronic scab; itching
Cutaneous SCC presents as an enlarging hyperkeratotic macule, scaly, or crusted lumps. They usually arise within pre-existing actinic keratosis or intraepidermal carcinoma
- They grow over weeks to months, they may ulcerate, and they are often tender or painful
- Located on sun-exposed sites, particularly the face, lips, ears, hands, forearms, and lower legs
- Size varies from a few millimeters to several centimeters in diameter
- On the exam, you will need to differentiate this from Basal Cell Carcinoma (look for telangiectasia of basal cell carcinoma central ulceration and rolled border) vs. scaly papules of SCC
DX: Diagnosis is by biopsy
TX: Treatment may involve Mohs surgery, radiation, medications, or in some cases chemotherapy
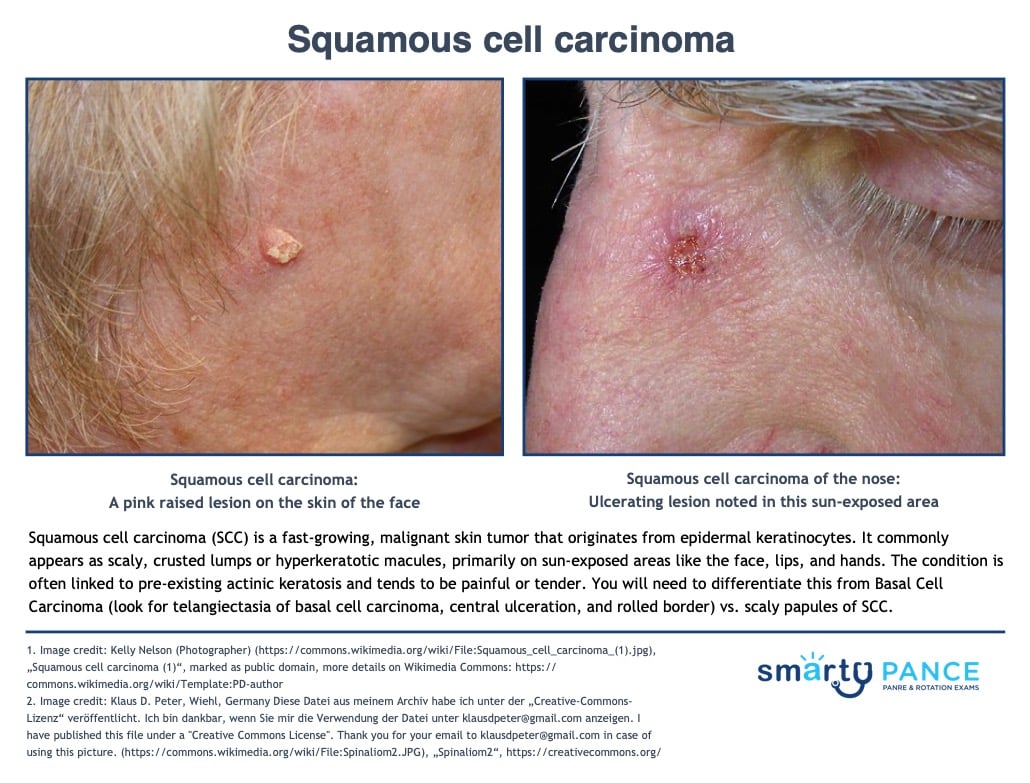
View more images of squamous cell carcinoma |
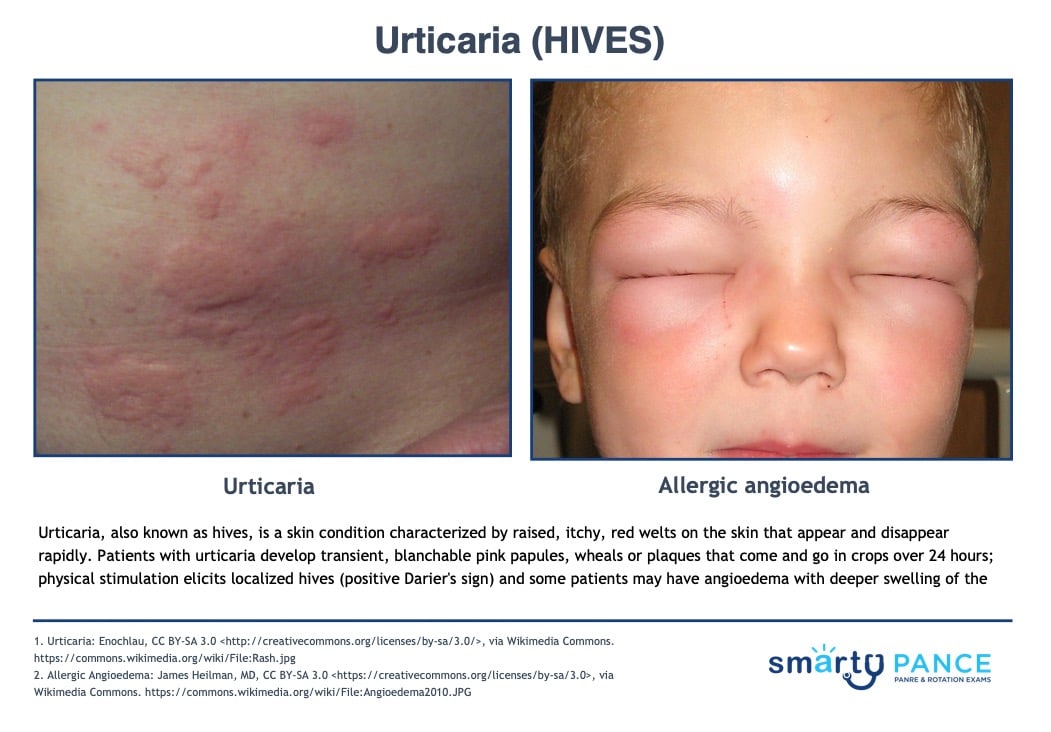
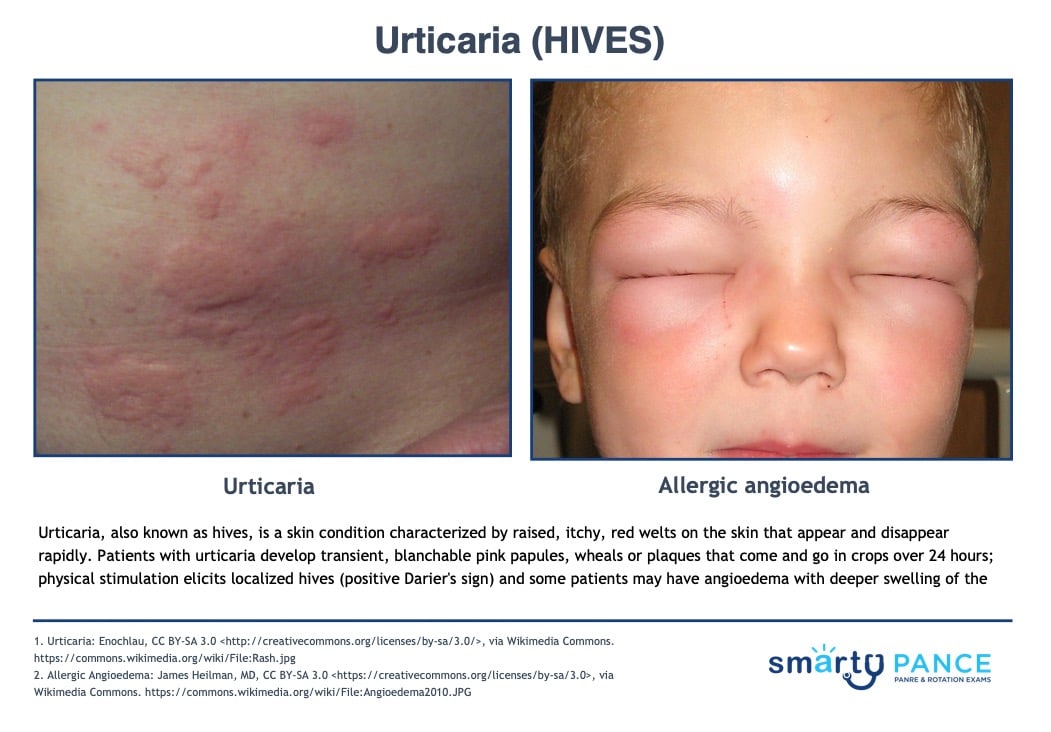
| Urticaria (postoperative) |
Urticaria (hives) is a skin rash triggered by a reaction to certain foods, medications, stress, or other irritants
- Symptoms include blanchable, pruritic, raised, red, or skin-colored papules, wheels, or plaques on the skin's surface
- (+) Darier's sign: localized urticaria appearing where the skin is rubbed (histamine release)
- Angioedema: a painless, deeper form of urticaria affecting the lips, tongue, eyelids hand and genital
Hives usually go away without treatment, but antihistamine medications are often helpful in improving symptoms
- If anaphylaxis give epinephrine: 0.3–0.5 mg; use 1:1,000 dilution for IM route and 1:10,000 for IV route
- Peds: epinephrine 0.01 mg/kg SC/IV
View more images of urticaria
|