Patient will present as → a 63-year-old male complaining of bilateral leg pain, which has been increasing gradually over the past several months. It worsens when he walks but improves with rest. Past medical and surgical history is significant for hypertension, hyperlipidemia, and coronary artery bypass graft (5 years ago). He has a 60-pack-year smoking history. Vital signs are as follows: Temp 37C, HR 70, BP 143/89, and RR 18. Physical exam of the lower extremities reveals palpable but weak posterior tibial and dorsalis pedis pulses bilaterally; they are warm and well-perfused. Ankle-brachial indices are 0.7 and 0.8.
Peripheral artery disease (PAD) is a circulatory condition in which narrowed blood vessels reduce blood flow to the limbs
- PAD is most commonly the result of atherosclerosis and is a significant independent risk factor for cardiovascular and cerebrovascular morbidity and mortality
- Lower extremity atherosclerotic PAD is initially asymptomatic but typically progresses to claudication, ischemia, and pain with exercise
- Acute arterial occlusion may be caused by thrombosis or embolism
- Thrombotic disease also may be a result of trauma, hypovolemia, inflammatory arteritis (including Takayasu arteritis and Buerger disease), polycythemia, dehydration, repeated arterial punctures, and hypercoagulable states
Intermittent claudication, foot or lower leg pain with exercise that is relieved by rest, is usually the first symptom of PAD. As the condition progresses, pain at rest develops.
- Femoral and distal pulses will be weak or absent; an aortic, iliac, or femoral bruit may be present.
- Skin changes to the lower extremity include loss of hair, shiny atrophic skin, and pallor with dependent rubor
- Severe, chronic disease results in numbness, tingling, and ischemic ulcerations, which may lead to gangrene.
- Acute arterial occlusion threatens limb viability and results in the “6 Ps”: pain, pallor, pulselessness, paresthesias, poikilothermia, and paralysis
| Disease | Pearls | Diagnostics | Treatment |
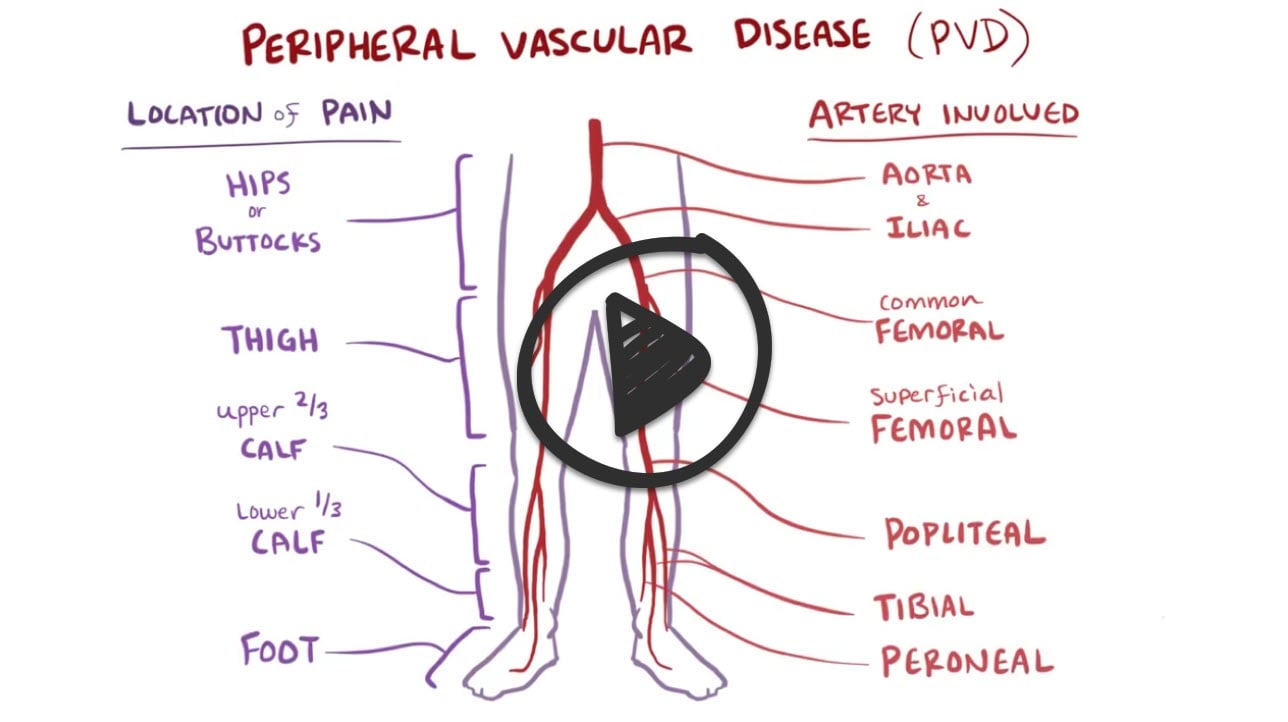
| Intermittent claudication | Occurs distal to the level of stenosis or occlusion
Physical
|
An ankle-brachial index (ABI), which uses Doppler measurements to compare the BP in the upper and lower extremities, is a highly sensitive and specific test
Angiography remains the gold-standard study
|
Stop smoking first line
Surgery
|
| Asymptomatic PAD | Screen patients with
Abnormal or absent pedal pulse Age > 7o Ages 50-69 with a history of smoking or DM |
Asymptomatic
Screen with ABI
|
Preventative treatment: ASA, lipid-lowering, blood pressure control |
| PAD or PVD | Occlusive atherosclerotic disease of lower extremities (noncardiac vessels)
Sites: superficial femoral artery (most common), popliteal, aortoiliac Risk factors: smoking, hyperlipidemia, DM, HTN Pain in one or more lower extremity muscle groups
Diminished or absent pulses
|
Lipids: hypercholesterolemia >240, hypertriglyceridemia >250
|
Prevention of atherosclerosis Control HLD, HTN, weight, DM
Manage primary hyperlipidemia: statins, diet, exercise Graduated exercise: walk to point of claudication, rest, then continue walking Foot care Reduce BP Stop smoking Most important Medical intervention:
Surgery:
Prognosis: Stable: 70%-80% Worsening: 10%- |
Doppler ultrasound flow studies can be used to determine systolic pressures in the peripheral arteries.
- An ankle-brachial index (ABI), which uses Doppler measures to compare the BP in the upper and lower extremities, is a highly sensitive and specific test
- An ABI of < 0.9 indicates significant disease
- Angiography remains the gold-standard study
- CT or magnetic resonance angiography is also useful for locating stenotic sites and for accurate diagnosis of thrombosis or embolism.
- Although not regularly used for screening, elevated homocysteine has a strong association with incidence and progression of PAD.
| ABI Value | Interpretation | Recommendation |
|---|---|---|
| Greater than 1.4 | Calcification/Vessel Hardening | Refer to vascular specialist |
| 1.0-1.4 | Normal | None |
| 0.9-1.0 | Acceptable | None |
| 0.8-0.9 | Some Arterial Disease | Treat risk factors |
| 0.5-0.8 | Moderate Arterial Disease | Refer to vascular specialist |
| Less than 0.5 | Severe Arterial Disease | Refer to vascular specialist |
Aggressive risk factor modification: Tobacco use must be discontinued; diabetes, HTN, and hyperlipidemia must be controlled
- Exercise - walking to the point of claudication
- Platelet inhibitors: cilostazol, aspirin, clopidogrel
- ACE inhibitors, statins, progressive exercise, and supervised exercise programs have been shown to be helpful at reducing symptoms of claudication
- If these interventions fail, revascularization with Percutaneous Transluminal Angioplasty (PTA), bypass grafts, and stenting
- Surgical graft bypass - reroute blood around blockages
- Angioplasty—balloon dilation
- Endarterectomy—remove diseased intima and media
- Surgical patch angioplasty (place patch over stenosis)
- Erectile dysfunction may require revascularization or treatment with a phosphodiesterase, such as sildenafil
 Osmosis Osmosis |
|
 |
Peripheral artery disease (PAD) is caused by the narrowing of peripheral arteries, especially those in the legs, due to plaque buildup. Patients with PAD can develop intermittent muscle cramping, arterial ulcers, critical limb ischemia, and paresthesias. If the condition is left untreated, amputation(s) may be necessary to remove the diseased limb(s).
Play Video + QuizQuestion 1 |
Thrombolysis Hint: Thrombolysis would be appropriate for a patient with an ischemic stroke. | |
Embolectomy | |
Fasciotomy Hint: A fasciotomy might be indicated after this patient's embolectomy, but would not be the initial management for this patient. | |
Amputation Hint: An amputation would be premature but may be indicated if the patient developed an infected limb. | |
No intervention necessary Hint: This patient has an intervenable condition; thus, an embolectomy would be indicated. |
Question 2 |
Elastic compression stockings Hint: Elastic compression stockings should be avoided as it can decrease arterial circulation to the skin. | |
Calcium channel blockers Hint: Calcium channel blockers have not proven to be beneficial. | |
Cilostazol | |
Warfarin Hint: Warfarin may prevent more cardiovascular events but causes more major bleeding and has not been shown to improve outcomes in those with chronic PAD. | |
Propranolol Hint: βblockers are contraindicated in isolated PAD as it will worsen claudication |
Question 3 |
Ankle/ brachial indices | |
MRI of the lumbar spine | |
Ultrasonography of the lower extremities | |
EMG of the lower extremities | |
Arteriogram of the lower extremities Hint: The use of arteriogram is not necessary unless the patient is considering surgery. |
|
List |
References: Merck Manual · UpToDate



