85 y/o male with back pain, left-sided abdominal pain, and no bowel movements for 7 days
Patient will present as → a 65-year-old male with chronic low back pain complaining of bloating, abdominal pain, straining, and pain with bowel movements. He reports less than 3 bowel movements per week that are very hard and difficult to pass. The patient is on 50 mcg of transdermal Fentanyl and takes four 10 mg Norco per day for breakthrough pain.
Definition of constipation
- According to the Rome III criteria, functional constipation is defined as any two of the following features:
- straining
- lumpy, hard stools
- a sensation of incomplete evacuation
- use of digital maneuvers
- a sensation of anorectal obstruction or blockage with 25 percent of bowel movements
- a decrease in stool frequency (less than three bowel movements per week)
The above criteria must be fulfilled for the last three months with symptom onset six months prior to diagnosis, loose stools should rarely be present without the use of laxatives, and there must be insufficient criteria for a diagnosis of irritable bowel syndrome.
- Patients who are older than 50 with new-onset constipation should be evaluated for colon cancer
- Bloating, abdominal pain, straining, and pain with bowel movements
- Opiate use is a classic cause of constipation. All patients on chronic opioids should be prophylaxed with a stool softener
- Think of causes of secondary causes of constipation: DM, hypothyroidism, MS, dehydration, and medications are common
Encopresis
A childhood condition characterized by recurrent soiling or passing of stool (often involuntarily) into clothing
- It typically occurs in children older than 4, after the age when they should have gained full bowel control
- On physical exam, you may note a distended or full-feeling abdomen and palpable mass in LLQ due to impacted stool
- A rectal exam could reveal a large amount of stool in the rectum
- Other signs might include anal fissures or skin irritation around the anus from recurrent soiling
- The treatment for encopresis involves clearing the bowel, maintaining regular stool softness, and promoting behavioral changes for consistent bowel movements
A comprehensive physical examination should be performed that includes a rectal exam to palpate for hard stool, assess for masses, anal fissures, hemorrhoids, sphincter tone, push effort during attempted defecation, prostatic hypertrophy in males, and posterior vaginal masses in females
- Imaging — There are limited data to support the role of imaging in the evaluation of constipation in the older adult
- Laboratory testing: CBC, CMP, TSH to identify secondary causes
Increase fiber (20-25 grams per day), exercise, and water in the diet
- The effects of fiber on bowel movements may take several weeks
- In a small study of healthy volunteers, the consumption of extra fluid was not associated with an increase in stool output
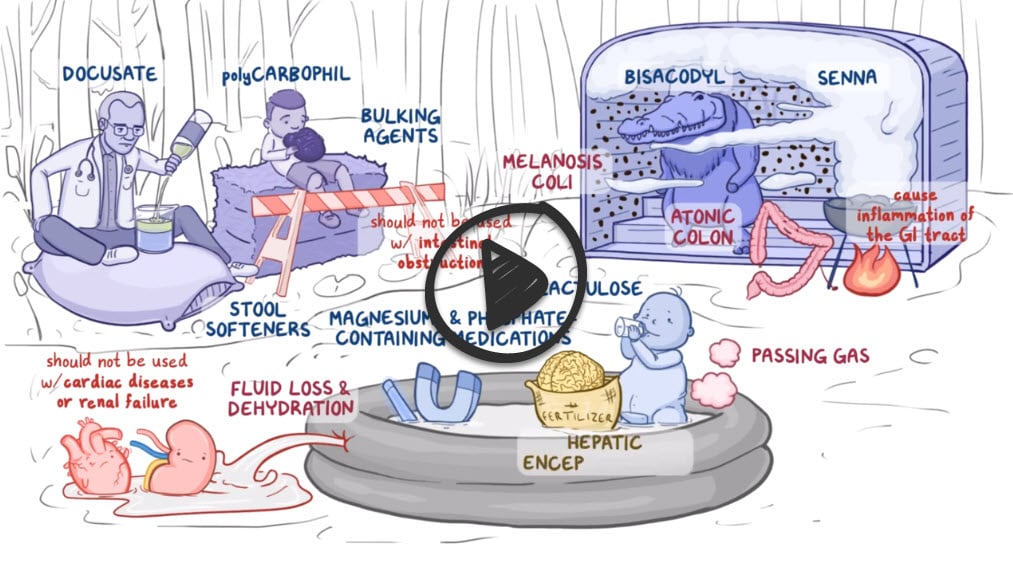
Laxatives: Laxative usage in older adults should be individualized based on the patient's history, comorbidities, drug interactions, and side effects.
- Bulk-forming laxatives first line — Bulk-forming laxatives include psyllium seed (eg, Metamucil), methylcellulose (eg, Citrucel), calcium polycarbophil (eg, FiberCon®), and wheat dextrin (eg, Benefiber)
- Osmotic laxatives can be used in patients not responding satisfactorily to bulking agents. Start with low-dose polyethylene glycol (PEG) as it has been demonstrated to be efficacious and well-tolerated in older adults
- Stimulant laxatives — Stimulant laxatives affect electrolyte transport across the intestinal mucosa and enhance colonic transport and motility
- Stool softeners, suppositories (glycerin or bisacodyl), and enemas have limited clinical efficacy and should only be used in specific clinical scenarios
- A patient with constipation lasting for more than 2 weeks that is refractory to treatments should undergo further investigation to identify the underlying cause
Question 1 |
Daily laxative Hint: This could be a suitable option for some patients, but long-term use of laxatives can lead to dependency and disrupt normal bowel function. | |
Regular enema Hint: Regular enemas are not typically recommended for managing chronic constipation due to the risk of bowel injury and electrolyte imbalances. | |
Increased fluid intake and high-fiber diet | |
Daily glycerin suppository Hint: Glycerin suppositories are generally safe for occasional use but are not typically recommended for long-term management of chronic constipation. | |
Surgical intervention Hint: Surgery is usually considered as a last resort when all other treatment options have failed and if there is a specific anatomical issue causing the constipation. In this case, the patient’s workup was negative, so surgery would not be the best next step. |
Question 2 |
Straining | |
Sensation of incomplete evacuation | |
Lumpy or hard stools | |
> 3 bowel movements per week |
Question 3 |
Opioids Hint: See answer C for explanation | |
Calcium channel blockers Hint: See answer C for explanation | |
Beta-blockers | |
NSAIDs Hint: See answer C for explanation |
Question 4 |
Loperamide | |
Docusate sodium Hint: Is a stool softener. It allows incorporation of water and fat into stools, causing stools to soften. It’s indicated for patients who should avoid straining during defecation. | |
Lactulose Hint: Is an osmotic laxative. It produces an osmotic effect in the colon resulting in bowel distention and stimulation of peristalsis. | |
Senna Hint: Is a stimulant laxative. It induces defecation by acting directly on the intestinal mucosa or nerve plexus, which stimulates peristaltic activity. |
Question 5 |
Parkinson’s disease Hint: See answer C for explanation | |
Colon cancer Hint: See answer C for explanation | |
Hirschsprung disease | |
Diverticular disease Hint: See answer C for explanation |
Question 6 |
Initiate a trial of over-the-counter laxatives Hint: While these can be used to manage constipation, the patient's age and rectal bleeding warrant further investigation before initiating treatment. | |
Repeat colonoscopy | |
Abdominal X-ray Hint: This can identify fecal impaction but is less useful in excluding serious underlying pathology. | |
Prescribe a high-fiber diet and increased fluid intake Hint: Although beneficial in managing constipation, it's important to first rule out serious pathology in this patient. | |
Stool softeners and osmotic laxatives Hint: These are treatment options, but the patient first needs a thorough evaluation due to his age and symptoms. |
|
List |
References: Merck Manual · UpToDate


 Osmosis
Osmosis