Patient will present with → a 3-year-old boy is brought to the clinic by his mother, who is concerned about his swollen belly and changes in his skin and hair color. The child lives in a resource-poor setting and has a diet primarily consisting of starchy foods with minimal protein. On examination, the child has a distended abdomen, generalized edema, and areas of hyperpigmentation and desquamation on his skin. His hair appears thin and has a reddish tint.
Patient will present with → a 3-year-old boy is brought to the clinic by his mother, who is concerned about his swollen belly and changes in his skin and hair color. The child lives in a resource-poor setting and has a diet primarily consisting of starchy foods with minimal protein. On examination, the child has a distended abdomen, generalized edema, and areas of hyperpigmentation and desquamation on his skin. His hair appears thin and has a reddish tint.
To watch this and all of Joe-Gilboy PA-C's video lessons, you must be a member. Members can log in here or join now.
According to the US Centers for Disease Control and Prevention, although less than 10% of the US population have nutritional deficiencies, those deficiencies vary by age, gender, and race, and the incidence may be 30% or higher among certain groups. One-half of all children worldwide (aged 6 months to 5 years) have one or more micronutrient deficiencies, with more than 2 billion people affected globally.
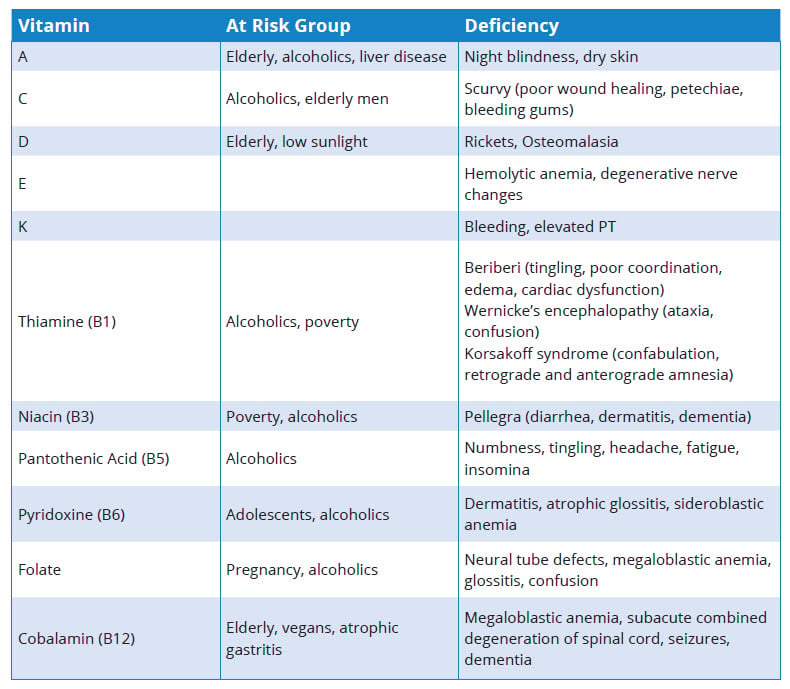
Here are some common nutritional deficiencies you are likely to see come exam day:
- Kwashiorkor is an inadequate intake of protein and may lead to edema in the abdomen, feet, and ankles
- Marasmus is inadequate intake of ALL energy forms (protein and calories) and leads to low body weight, wasting of muscle and fat, skin that is dry and wrinkled, and hair that is thin and brittle
- Fat-Soluble Vitamins (ADEK):
- Vitamin A: Elderly, alcoholics, liver disease - night blindness, dry skin
- Vitamin D: Elderly, low sunlight - rickets, osteomalacia
- Symptoms of Vitamin D deficiency can include fatigue, bone or muscle pain, proximal muscle weakness, mood changes, and slow wound healing
- Certain medications can cause vitamin D deficiency - seizure medications (such as phenytoin therapy), steroids, isoniazid and rifampin for tuberculosis, antiretrovirals (ritonavir), cancer treatments (taxol and cyclophosphamide, estrogen blockers (tamoxifen), and others
- Vitamin E: neuropathy, ataxia
- Vitamin K: bleeding (makes clotting factors - causes an increase in PT/INR)
- Vitamin C: Alcoholics, elderly men - scurvy (swollen gums, bruising, petechiae, hemarthrosis, anemia, poor wound healing, perifollicular and subperiosteal hemorrhages, and corkscrew hair)
- Thiamine (B1): Alcoholics, poverty - Beriberi (tingling, poor coordination, edema, cardiac dysfunction).Wernicke’s encephalopathy (ataxia, confusion). Korsakoff syndrome (confabulation, retrograde, and anterograde amnesia)
- Niacin (B3): Poverty, alcoholics - Pellagra (diarrhea, dermatitis, dementia).
- Pantothenic Acid (B5): Alcoholics - Numbness, tingling, headache, fatigue, insomnia.
- Pyridoxine (B6): Adolescents, alcoholics - Dermatitis, atrophic glossitis, sideroblastic anemia.
- Folate: Pregnancy, alcoholics - Neural tube defects, megaloblastic anemia, glossitis, confusion.
- Cobalamin (B12): Elderly, vegans, atrophic gastritis - Megaloblastic anemia, subacute combined degeneration of spinal cord, seizures, dementia.
Nutritional Deficiencies
Order appropriate laboratory studies based on suspected deficiency
Vitamin replacement/supplementation
- Address (and fix) underlying cause
| Picmonic | |
 |
Zinc deficiency is marked by a variety of symptoms due to the fact that zinc is an essential metallic element used in over 100 enzymatic reactions. Zinc is commonly used as a stabilizer in a small protein structural motif called a zinc finger that is commonly used for binding DNA and RNA as transcription factors. Zinc deficiency can present in a multitude of ways including changes in smell, taste, hair growth, wound healing as well as hypogonadism and a perioral rash. A common population with this deficiency is severe alcoholics due to poor nutritional intake and poor absorption. Play Video + Quiz |
 |
Wernicke-Korsakoff syndrome is a common acute neuropsychological disorder caused by thiamine deficiency. It is commonly seen in alcoholics due to nutrient depletion. Wernicke encephalopathy is manifested by a clinical triad of encephalopathy with confusion, ophthalmoplegia, and gait ataxia. Korsakoff syndrome is characterized by marked deficits in anterograde and retrograde memory, personality changes, and confabulation. Memory impairment correlates with damage to the medial dorsal nucleus of the thalamus and the mamillary bodies. Patients with Korsakoff syndrome rarely recover. When treating alcoholics, thiamine is commonly given with glucose therapy to prevent development of Wernicke-Korsakoff syndrome. Play Video + Quiz |
 |
Vitamin K is a fat soluble vitamin, which is synthesized to an active form by the gut flora and the actions of the enzyme epoxide reductase. The active form plays a role in the carboxylation of glutamate, which is an essential reaction in the synthesis of blood clotting factors II, VII, IX, X, protein C and protein S. Without the synthesis of these proteins, the patient has severely impaired blood clotting. This can be seen in patients with a vitamin K deficiency or who are on warfarin therapy, which is a vitamin K antagonist. Common causes of vitamin K deficiency include malabsorption, as well as gut flora depletion, which is seen in neonates and in patients with prolonged antibiotic use. Those who are vitamin K deficient will display a normal bleeding time with increased PT and PTT. Play Video + Quiz |
 |
Vitamin E is a fat-soluble vitamin that functions biologically as an antioxidant. Important biologic functions of this vitamin, which include the compounds tocopherols and tocotrienols, include disabling free radicals in the body, inhibiting platelet aggregation, promoting cell repair, and smooth muscle growth. Deficiencies in vitamin E can be caused by fat malabsorptive disorders, which include cystic fibrosis, Whipple’s disease, and celiac disease, among others. Deficiency of this vitamin leads to hemolytic anemia, spinocerebellar ataxia, peripheral neuropathy, ataxia, myopathies and impaired immune response. Those deficient in vitamin E are also prone to the development of hyperkeratosis and acanthosis nigricans. Play Video + Quiz |
 |
Vitamin D is a fat-soluble vitamin whose major function is the maintenance of adequate levels of calcium and phosphorous in the body. There are several causes for vitamin D deficiency including renal failure, inadequate exposure to sunlight, fat malabsorption, and chronic liver disease. Children that are strictly breastfed are also at high risk for vitamin D deficiency because there are decreased levels in breast milk. There are several manifestations of vitamin D deficiency including rickets in children whose epiphyses have not closed, osteomalacia in adults, and hypocalcemic tetany. Play Video + Quiz |
 |
Vitamin C, also called ascorbic acid, is a water-soluble vitamin which is mostly essential for collagen synthesis and its antioxidant properties. The vitamin catalyzes several enzymes in the synthesis of collagen as well as catecholamine synthesis. When the vitamin is deficient, the most notable effect is the onset of Scurvy, a disease characterized by poor wound healing and perifollicular hemorrhage. Additionally, patients deficient in the vitamin can have anemia due to poor antioxidant ability as well as iron absorption problems. Play Video + Quiz |
 |
Vitamin B6 is a water-soluble vitamin that is activated to form pyridoxal phosphate, a cofactor in many reactions in body. This cofactor is used in multiple reactions of amino acid metabolism, including transamination and decarboxylation. Pyridoxal phosphate is also necessary for glycogen phosphorylase, cystathionine synthesis, heme synthesis, and the conversion of tryptophan to niacin. Vitamin B6 deficiency can cause low activity of these enzymes and lead to symptoms of hyperirritability, seizures, peripheral neuropathy, and sideroblastic anemia. Play Video + Quiz |
 |
Vitamin B5 is a water-soluble vitamin, also called pantothenic acid. This vitamin is essential for the synthesis of coenzyme A. Its utilization as a cofactor is essential for pyruvate dehydrogenase and fatty acid synthase, which are needed for glucose metabolism and fatty acid synthesis, respectively. A deficiency can present with non-specific signs of alopecia, dermatitis and enteritis. Additionally, the vitamin deficiency can result in adrenal insufficiency due to its role in fatty acid and hormone synthesis. Play Video + Quiz |
 |
Niacin, vitamin B3, is an essential vitamin used in energy reactions as a component of NAD. Niacin is created from the amino acid tryptophan and requires vitamin B6 in order to convert the amino acid to niacin. There is a characteristic set of symptoms referred to as pellagra which results from niacin deficiency. The symptoms of pellagra are easily remembered as the 4 D's which include diarrhea, dermatitis, dementia and death. Niacin deficiency often results from depletion of tryptophan as is seen in Hartnup disease and serotonin syndrome. Additionally, niacin can be used as a cholesterol lowering medication. As a medication, its most significant side effect is a facial flush. Play Video + Quiz |
 |
Vitamin B12, also called cobalamin, is a water-soluble vitamin with an essential role in the normal functioning of the nervous system and proper formation of blood cells. Vitamin B12 is found in foods that come from animals and is stored largely in the liver. It is involved in cellular functions in every cell of the body including roles in DNA synthesis, fatty acid synthesis and energy production. Vitamin B12 dependent enzymes including methylmalonyl Coenzyme A mutase, which converts methylmalonyl CoA to succinyl CoA and methionine synthase, which converts homocysteine to methionine. A vitamin B12 deficiency will hinder these reactions. Inability to convert homocysteine to methionine causes poor DNA synthesis and can cause macrocytic megaloblastic anemia with hypersegmented neutrophils. This can also be seen in a folate deficiency, which is also necessary to complete this reaction. However, a vitamin B12 deficiency will uniquely cause defects to the nervous system because elevated levels of methylmalonic acid can cause abnormal fatty acids to be incorporated into myelin, resulting in demyelination. This often causes damages to specific neuron tracts including the posterior columns, lateral corticospinal tract, and spinocerebellar tracts. Play Video + Quiz |
 |
Vitamin A, also called retinol, is an important vitamin that plays a role in a variety of functions throughout the body including, vision and skin health. This vitamin is needed by the retina of the eye for low-light and color vision. Therefore, night blindness is one of the first symptoms of vitamin A deficiency. Vitamin A in the form of retinoic acid is also important in the maintenance of normal skin healthy by activating genes and differentiating immature keratinocyte skin cells into mature epidermal cells. Therefore, skin changes like dry skin is often a sign of vitamin A deficiency. This vitamin also plays roles in gene transcription, immune function, embryonic development and has antioxidant activity. Play Video + Quiz |
 |
Thiamine, also called vitamin B1, is a water-soluble vitamin that is involved in many cellular processes. In biochemistry, thiamine is most commonly seen in the phosphate derivative form thiamine pyrophosphate (TPP). This coenzyme is necessary in the proper functioning of essential enzymes in the catabolism of sugars and amino acids including branched chain amino acid dehydrogenase, pyruvate dehydrogenase, alpha ketoglutarate dehydrogenase, and transketolase. Because these enzymes are used to make ATP for cellular energy, thiamine depletion can cause severe ATP depletion. Symptoms of thiamine deficiency have a broad range including Wernicke-Korsakoff syndrome and beriberi. In general, aerobic tissues that require high levels of ATP for proper functioning like the brain and heart are affected first. Because thiamine is necessary for glucose metabolism, infusion of glucose can precipitate or worsen thiamine deficiency. Therefore, thiamine is always given with IV glucose in patients susceptible to a thiamine deficiency. Play Video + Quiz |
 |
Riboflavin, also known as vitamin B2, is a water soluble vitamin that is the central component of cofactors FAD and FMN. FAD (flavin adenine dinucleotide) is a cofactor involved in several redox reactions and can be reduced to FADH2 when it accepts two hydrogen atoms. This reaction is especially important in the citric acid cycle as FAD is a prosthetic group in the enzyme complex succinate dehydrogenase. FAD is reduced to FADH2 as succinate is oxidized to fumarate and the high-energy electrons are sent through the electron transport chain to produce 2 ATP. It is important to note that FADH2 can only produce 2 ATP as compared to NADH2, which can make 3 ATP through the electron transport chain. In humans, signs and symptoms of a riboflavin deficiency include cracked lips, inflammation of the lining of the mouth, and cracks at the corners of the mouth. The eyes may also become bloodshot, itchy, watery and sensitive to bright light. Play Video + Quiz |
 |
Iron (Ferrous Sulfate) is an inexpensive drug of choice for treating and preventing iron deficiency anemia. The administration of iron promotes hemoglobin production necessary for carrying oxygen throughout the body. Ferrous sulfate is indicated for treating iron deficiency anemia. Side effects include constipation, diarrhea, nausea, vomiting, and dark green or black colored stools. Instruct the patient to take this medication with food and avoid concurrent antacid use. Teach the patient about measures to prevent liquid preparations from staining teeth and to keep this medication out of reach of children. This medication may worsen GI symptoms and should be used with caution in patients with peptic ulcers, ulcerative colitis, and regional enteritis. Play Video + Quiz |
 |
Folate deficiency occurs due to malabsorption, insufficient dietary intake, impaired metabolism and increased requirements for folate. It results in a macrocytic, megaloblastic anemia similar to Vitamin B12 deficiency; however, unlike Vitamin B12 deficiency it does not result in neurologic symptoms. Play Video + Quiz |
 |
Vitamin D2 can be obtained through diet, or synthesized in the body with exposure to sunlight. This vitamin acts like a hormone in the body, regulating calcium and phosphorous levels in the blood. Because it is controlled by a negative feedback loop, levels of vitamin D will increase when calcium is low and decrease when the calcium level returns to normal limits. Signs and symptoms of vitamin D toxicity, also known as hypervitaminosis D, are closely associated with hypercalcemia, which occurs more often in children. These include fatigue, muscle weakness, constipation, and kidney stones. Vitamin D supplementation is indicated in the treatment of hyperparathyroidism, rickets, and hypophosphatemia. Play Video + Quiz |
 |
Cholecalciferol (vitamin D3) is a key nutrient for bone health and made in the skin through sunlight exposure. Other sources of vitamin D3 include fortified milk and dietary supplements. Vitamin D3 supplementation is indicated as a prophylaxis and treatment for vitamin D deficiency. Symptoms of vitamin D deficiency include fatigue, constipation, hypercalcemia, and kidney stones. Compared with ergocalciferol (vitamin D2), vitamin D3 is more effective at raising serum levels of vitamin D (refer to the Picmonic on "Ergocalciferol (Vitamin D2)"). Excessive intake of vitamin D is toxic and may lead to hypervitaminosis D. Accidental vitamin D poisoning in children and adults requires medical attention. Play Video + Quiz |
 |
Biotin (vitamin B7) deficiency typically presents with alopecia, dermatitis and non-specific enteritis. Biotin is an essential cofactor in carboxylation reactions which are synthetic reactions used in fatty acid and amino acid synthesis. Classic causes of biotin deficiency are long-term antibiotic use as well as ingestion of raw eggs. Raw eggs contain a compound called avidin which binds the biotin and inactivates it. Play Video + Quiz |
 |
Beriberi develops due to thiamine (B1) deficiency. Beriberi is described as dry or wet. Dry beriberi is characterized by symmetric polyneuritis affecting both sensory and motor components of the distal extremities leading to symmetrical extremity muscle wasting. Wet beriberi has additional cardiac involvement including cardiomegaly, dilated cardiomyopathy, congestive heart failure, and peripheral edema. Play Video + Quiz |
Question 1 |
Protein deficiency only | |
Energy deficiency only Hint: See A for explanation | |
Combined protein and energy deficiency Hint: Causes Marasmus. | |
None of the above |
Question 2 |
Thiamine deficiency | |
Niacin deficiency Hint: See A for explanation | |
Vitamin A deficiency Hint: See A for explanation | |
Cobalamin deficiency Hint: See A for explanation |
Question 3 |
Nystagmus Hint: See B for explanation | |
Amnesia | |
Truncal ataxia Hint: See B for explanation | |
Confusion Hint: See B for explanation |
Question 4 |
Dermatitis Hint: See D for explanation | |
Diarrhea Hint: See D for explanation | |
Dementia Hint: See D for explanation | |
Diabetes |
Question 5 |
Vitamin B | |
Vitamin K Hint: Fat soluble vitamins are vitamins A, D, E, and K. Their absorption is affected in fat malabsorption. | |
Vitamin D Hint: Fat soluble vitamins are vitamins A, D, E, and K. Their absorption is affected in fat malabsorption. | |
Vitamin A Hint: Fat soluble vitamins are vitamins A, D, E, and K. Their absorption is affected in fat malabsorption. | |
Vitamin E Hint: Fat soluble vitamins are vitamins A, D, E, and K. Their absorption is affected in fat malabsorption. |
Question 6 |
Dry skin | |
Diffuse thyroid enlargement | |
Periorbital edema | |
Delayed relaxation phase of the deep tendon reflexes |
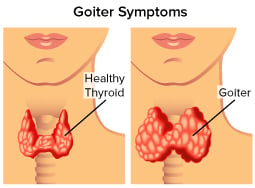 Patients with iodine deficiency tend to come from regions where iodine deficiency disorders are endemic. The first sign of iodine deficiency is diffuse thyroid enlargement, which becomes multinodular over time. In patients with hypothyroidism due to severe iodine deficiency, one might see such signs as dry skin, periorbital edema, and delayed relaxation phase of the deep tendon reflexes.
Patients with iodine deficiency tend to come from regions where iodine deficiency disorders are endemic. The first sign of iodine deficiency is diffuse thyroid enlargement, which becomes multinodular over time. In patients with hypothyroidism due to severe iodine deficiency, one might see such signs as dry skin, periorbital edema, and delayed relaxation phase of the deep tendon reflexes.Question 7 |
Hematologic Hint: See B for explanation | |
Cardiovascular | |
Genitourinary Hint: See B for explanation | |
Gastrointestinal Hint: See B for explanation |
- Nonspecific T-wave changes: U waves
- Prolonged QT and QU interval
- Repolarization alternans
- Premature ventricular contractions: monomorphic ventricular tachycardia
- Torsade de pointes
- Ventricular fibrillation
- Enhanced digitalis toxicity
Question 8 |
Pregnant women should receive routine vitamin A supplementation | |
A serum retinol-binding protein (RBP) study is the criterion standard for diagnosis of vitamin A deficiency
| |
Individuals with vitamin A deficiency may have a recent history of increased infections and/or infertility | |
Reduction in mortality and morbidity is seen in children aged 1-6 months who receive vitamin A supplementation |
Question 9 |
Most cases of hypocalcemia are detected owing to clinical findings during physical examination Hint: Most cases of hypocalcemia are discovered by clinical suspicion and appropriate laboratory testing. | |
Parathyroid hormone (PTH) should be measured after other routine laboratory measurements and after imaging studies have been conducted Hint: The PTH level should be checked as early as possible. Low to normal PTH levels occur in patients with hereditary or acquired hypoparathyroidism and in patients with severe hypomagnesemia. | |
Blood urea nitrogen (BUN) and serum creatinine levels are typically decreased in patients with calcium deficiency Hint: BUN and serum creatinine levels should be measured, because elevated levels may indicate renal dysfunction. | |
Serum albumin measurement is required to distinguish true hypocalcemia from factitious hypocalcemia |
Question 10 |
Treatment should aim to bring serum 25(OH)D levels above 30-32 ng/mL, which is the level at which calcium absorption is optimized | |
Routine screening to determine the need for vitamin D supplementation is indicated in most children and elderly persons | |
Many vegetables are a good source of vitamin D | |
Ingested vitamin D and vitamin D from sun exposure last the same length of time in the blood |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture