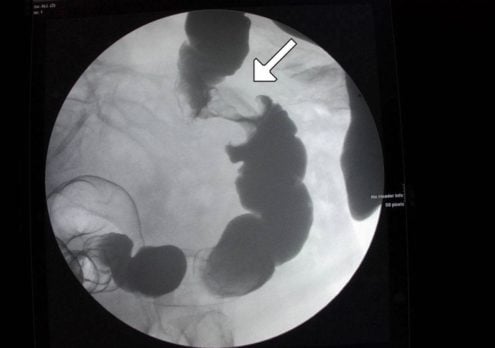
Patient will present as → a 68-year-old male presents with a 6-month history of progressive fatigue and a change in bowel habits, including intermittent diarrhea and constipation. He also reports unintentional weight loss of 10 pounds over the last three months. He has a history of smoking but no significant family history of cancer. On examination, he appears pale, and digital rectal examination reveals occult blood. Laboratory tests show iron deficiency anemia and mildly elevated ALT and AST. A colonoscopy is performed, revealing a mass in the descending colon, and a biopsy confirms adenocarcinoma. CT scans are ordered for staging. The patient is referred to an oncologist for further management, including potential surgical resection and adjuvant chemotherapy.
To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Progression of adenomatous polyp into malignancy (adenocarcinoma) usually occurs within 10-20 years - Colon CA is the third leading cause of cancer death after lung cancer and skin cancer
- Risk factors include age > 45 y/o, inflammatory bowel disease, polyps, low fiber, high animal fat diet, smoking, ETOH
- Presents as painless rectal bleeding and a change in bowel habits
- Selectively screen adults aged 76 to 85 years for colorectal cancer:
- There is adequate evidence that the benefits of detection and early intervention decline after age 75 years
- Discuss together with patients the decision to screen, taking into consideration the patient’s overall health status (life expectancy, comorbid conditions), prior screening history, and preferences.
Recommended intervals for colorectal cancer screening tests include:
Stool tests:
- High-sensitivity gFOBT or FIT every year
- sDNA-FIT every 1 to 3 years
CT colonography every 5 years
-
- (1 additional individual per 1000 would develop cancer in his or her lifetime due to radiation exposure)
Flexible sigmoidoscopy every 5 years or flexible sigmoidoscopy every 10 years + FIT every year
- (Serious complications occur in approximately 3.4 per 10,000 procedures)
Colonoscopy screening every 10 years
-
- Perforation of the colon occurs in an estimated 3.8 per 10,000 procedures
- Serious complications—including perforation, major bleeding, diverticulitis, severe abdominal pain, and cardiovascular events occur in an estimated 25 per 10,000 procedures
USPSTF colorectal cancer screening guidelines
**When adequate screening colonoscopy is accomplished, intercurrent stool tests (i.e., between colonoscopy examinations) are not necessary. In addition, for patients who have had a negative colonoscopy and have been recommended to have routine screening in 10 years, screening with FIT or other screening tests is not indicated prior to the end of the 10-year period.
"Hereditary factors are believed to contribute to up to 30% of colorectal cancers. Relative risk is 3.8 times if the family member's cancer was diagnosed at less than 45 years of age. Recommended screening in a single first-degree relative with colorectal cancer diagnosed before age 60 is beginning colonoscopy at age 40 or ten years younger than the age at diagnosis of the youngest affected first-degree relative. Then if negative, every 5 years."
Treatment is surgical resection and chemotherapy for nodal involvement
- 5FU is mainstay of chemotherapy
- Monitor CEA with treatment
 Osmosis Osmosis |
|
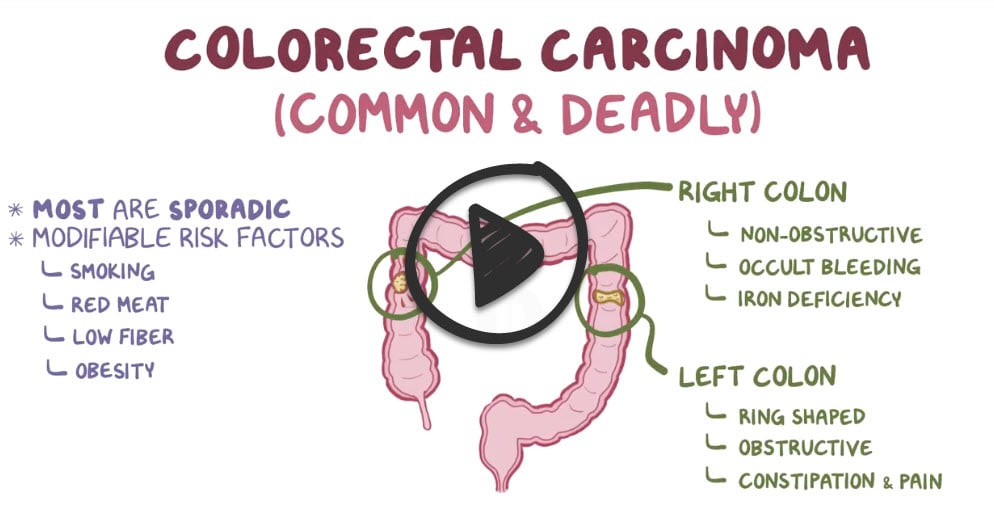 |
Colorectal cancer is the third most common cancer in both men and women with the majority of cases being adenocarcinoma. Risk factors include a family history of colorectal cancer, personal history of inflammatory bowel diseases such as ulcerative colitis or Crohn’s disease, a diet high in red meat, obesity, alcohol consumption greater than four drinks per week, and cigarette smoking. Clinical manifestations of early-stage colorectal cancer are usually non-specific, while manifestations of late-stage colorectal cancer include hepatomegaly, peritonitis, and abdominal pain. Patients aged 45 and older should undergo a colonoscopy once every 10 years to assess for polyps and/or the presence of cancer.
Play Video + QuizQuestion 1 |
Repeat colonoscopy in one year Hint: Inappropriate given the current findings suggestive of cancer. | |
Immediate initiation of chemotherapy Hint: Premature without a histological diagnosis. | |
Biopsy of the mass during colonoscopy | |
Surgical resection of the mass without biopsy Hint: Histological diagnosis is essential before definitive surgery for cancer. | |
Prescription of a high-fiber diet Hint: While beneficial for overall colon health, it is not a treatment for colon cancer. |
Question 2 |
Palliative care only Hint: Indicated for advanced, non-curable cancers, not for localized stage II disease. | |
Chemotherapy alone Hint: Not the standard initial treatment for localized colon cancer, which is amenable to surgery. | |
Radiation therapy alone Hint: More commonly used for rectal cancer, not standard for colon cancer. | |
Surgical resection followed by adjuvant chemotherapy based on risk factors | |
Immunotherapy Hint: urrently, it is used in specific contexts, such as mismatch repair-deficient/microsatellite instability-high (dMMR/MSI-H) colon cancers, not broadly for all stage II cases. |
Question 3 |
Adenomatous Polyp | |
Inflammatory Polyp Hint: While inflammatory polyps can occur in the setting of conditions like ulcerative colitis, which has an increased risk for colon cancer, they are not the most common precursor to carcinoma of the colon. | |
Hyperplastic Polyp Hint: Hyperplastic polyps are generally considered to have a very low risk of progressing to cancer and are not the typical origin of colon carcinomas. | |
Benign Lymphoid Polyp Hint: These polyps are relatively rare and not commonly associated with the development of colon cancer. | |
Hamartomatous Polyp Hint: Although hamartomatous polyps can be part of syndromes that increase cancer risk (like Peutz-Jeghers syndrome), they are not the most frequent source of colon carcinomas compared to adenomatous polyps. |
Question 4 |
5% Hint: See D for explanation | |
10% Hint: See D for explanation | |
15% Hint: See D for explanation | |
25% |
Question 5 |
There is good evidence to include stool-based testing in screening asymptomatic patients older than 45 years for colorectal carcinoma | |
There is fair evidence to include stool-based testing in screening asymptomatic patients older than 45 years for colorectal carcinoma Hint: This statement underestimates the level of evidence and recommendation strength provided by current guidelines and research findings, which classify the evidence as good. | |
There is insufficient evidence to include or to exclude stool-based testing testing as an effective screening test for colorectal cancer in asymptomatic patients older than 45 years Hint: This statement is incorrect. There is sufficient evidence from randomized controlled trials and observational studies that support the effectiveness of stool-based testing in reducing colorectal cancer mortality. | |
Stool-based testing has been shown to increase the risk of colorectal cancer in asymptomatic patients older than 45 years. Hint: This statement is false. There is no evidence to suggest that stool-based testing increases the risk of colorectal cancer. On the contrary, these tests are used to detect hidden blood in the stool, which can be an early sign of cancer, thereby potentially reducing the risk of advanced colorectal cancer through early detection and treatment. | |
None of the above. Hint: This option is incorrect because statement A accurately describes the current evidence supporting the use of fecal occult blood screening for colorectal cancer. |
Question 6 |
CEA is a cost-effective screening test for colorectal cancer Hint: See B for explanation | |
elevated preoperative CEA levels correlate well with postoperative recurrence rate in colorectal cancer | |
CEA is a sensitive test for colorectal cancer Hint: See B for explanation | |
CEA is a specific test for colorectal cancer Hint: See B for explanation | |
CEA has no value in predicting recurrence in colorectal cancer
Hint: See B for explanation |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture