The NCCPA™ Gastroenterology and Nutrition PANCE Content Blueprint gastrointestinal system neoplasms (PEARLS)
| Esophageal Neoplasms | Patient will present as → a 62-year-old man with a history of alcoholism who complains of difficulty swallowing solids that has progressed to difficulty swallowing liquids. He has smoked 1-2 packs of cigarettes per day for the past 38 years. In addition, he reports occasional bouts of hematemesis and hoarseness, along with progressive weight loss and weakness. Progressive dysphagia to solid foods along with weight loss, reflux, and hematemesis
Adenocarcinoma:
Squamous cell:
DX: endoscopy + biopsy TX: Resection |
| Gastric Neoplasms | Patient will present as → a 58-year-old male chef with a history of smoking and chronic gastritis presents with a four-month history of progressive epigastric pain, occasional vomiting, and a 15-pound weight loss. He reports the pain worsens after eating, especially with spicy foods. Recently, he noticed decreased appetite and early satiety. He has no family history of gastrointestinal cancers. Physical examination reveals mild epigastric tenderness without palpable masses. You are surprised to discover a firm, enlarged, painless lymph node above the patient’s left clavicle. Laboratory tests show Guiac-positive stool and iron deficiency anemia. An upper endoscopy reveals a 3 cm ulcerated lesion in the antrum of the stomach, and a biopsy confirms adenocarcinoma. Abdominal pain and unexplained weight loss are the most common symptoms, along with reduced appetite, anorexia, dyspepsia, early satiety, nausea and vomiting, anemia, melena, and guaiac-positive stool
DX: Upper endoscopy with biopsy
Treatment: Gastrectomy, radiotherapy, chemotherapy; poor prognosis |
| Liver neoplasms (ReelDx) | ReelDx Virtual Rounds (Liver neoplasms)Patient will present as → a 52-year-old female with a history of cirrhosis secondary to long-standing alcohol abuse visits your office to discuss a 15-pound weight loss over the last 6 months. She reports early satiety, jaundice, and vague abdominal discomfort. Her ascites, generally stable and small, has worsened in the last 3 weeks. Abdominal pain, weight loss, right upper quadrant mass
DX:
TX: Resection, transplant - poor prognosis |
| Pancreatic neoplasms (ReelDx) | ReelDx Virtual Rounds (Pancreatic neoplasms)Patient will present as → a 68-year-old smoker with a 25 lb weight loss over the last three months that is associated with a burning pain deep in the epigastrium after eating, diarrhea, and jaundice. Physical exam reveals a palpable, non-tender gallbladder and clay-colored stool. Labs show a total bilirubin of 8, alkaline phosphatase of 450, and an ALT of 150. Painless jaundice is pathognomonic!
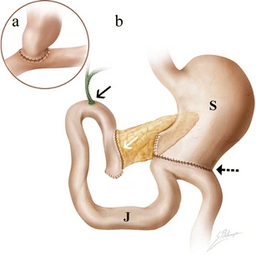
DX: Diagnose with abdominal CT scan - 75% show tumor at the head of the pancreas, 25% at the tail
Treatment: Whipple procedure: remove the antrum of the stomach, part of the duodenum, head of the pancreas, gallbladder |
| Colon cancer | Patient will present as → a 68-year-old male presents with a 6-month history of progressive fatigue and a change in bowel habits, including intermittent diarrhea and constipation. He also reports unintentional weight loss of 10 pounds over the last three months. He has a history of smoking but no significant family history of cancer. On examination, he appears pale, and digital rectal examination reveals occult blood. Laboratory tests show iron deficiency anemia and mildly elevated ALT and AST. A colonoscopy is performed, revealing a mass in the descending colon, and a biopsy confirms adenocarcinoma. CT scans are ordered for staging. The patient is referred to an oncologist for further management, including potential surgical resection and adjuvant chemotherapy. Painless rectal bleeding and a change in bowel habits in a patient 50-80 years of age
Screening begins at 45 and continues until 75 y/o
Recommended intervals for colorectal cancer screening tests include
Selectively screen adults aged 76 to 85 years for colorectal cancer:
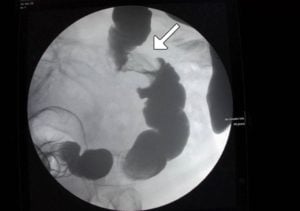
DX: Definitive diagnosis is with colonoscopy and biopsy. Barium enema will classically show an "apple core lesion"
Treatment: Resect tumors and adjuvant chemotherapy |
| Anorectal cancer | Patient will present as → a 69-year-old male who complains of rectal pruritus, bleeding with defecation, and a sensation of incomplete evacuation. A palpable mass is noted on digital rectal examination. Rectal bleeding + tenesmus (a feeling of incomplete emptying after a bowel movement), the most common anorectal cancer is adenocarcinoma
DX: Typically, colonoscopy is done whenever rectal bleeding occurs, even in patients with obvious hemorrhoids or known diverticular disease. Coexisting cancer must be ruled out TX: Treated with wide local surgical excision, radiation with chemotherapy for large tumors with metastases |