To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
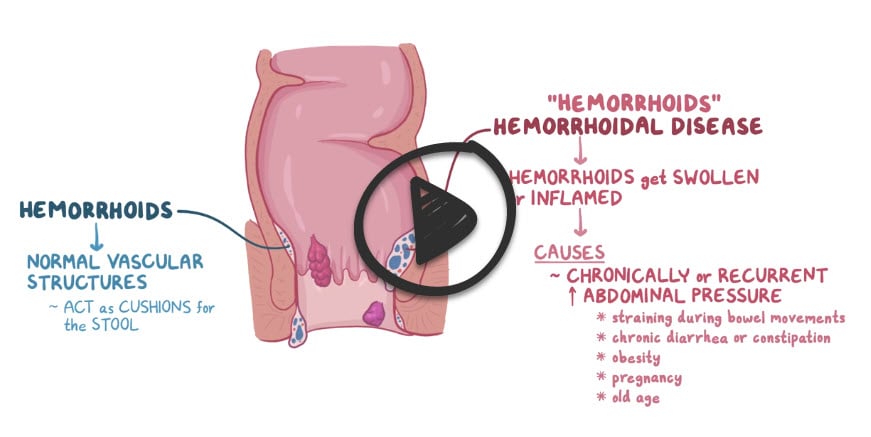
Hemorrhoids are swollen and inflamed veins in the rectum and anus that cause discomfort and bleeding
- Hemorrhoids are usually caused by straining during bowel movements, obesity, or pregnancy
- Discomfort is a common symptom, especially during bowel movements or when sitting. Other symptoms include itching and bleeding
There are three types of hemorrhoids
- External hemorrhoids are distal to the dentate line
- Internal hemorrhoids are proximal to the dentate line
- Mixed hemorrhoids are located both proximal and distal to the dentate line
Internal hemorrhoids (above the dentate line): no pain, but bright red blood per rectum
- Internal hemorrhoids typically manifest with bleeding after defecation; blood is noted on toilet tissue and sometimes in the toilet bowl
- Internal hemorrhoids may be uncomfortable but are not as painful as thrombosed external hemorrhoids
- Internal hemorrhoids sometimes cause mucus discharge and a sensation of incomplete evacuation
External hemorrhoids (below dentate line): Pain, but no bleeding
- External hemorrhoids may become thrombosed, resulting in painful, purplish swelling
- Rarely they ulcerate and cause minor bleeding. Cleansing the anal region may be difficult
Strangulated hemorrhoids occur when protrusion and constriction occlude the blood supply. They cause pain that is occasionally followed by necrosis and ulceration.
Physical examination
- Inspection of the anal verge and perianal area for external hemorrhoids, prolapsed internal hemorrhoids, or other possible causes of anal symptoms (e.g., condylomata)
- Digital rectal examination (DRE) for palpation for masses, tenderness, and characterization of anal sphincter tone
Studies
- Anoscopy is indicated in patients where hemorrhoids were not detected on physical examination and DRE
- Colonoscopy/flexible sigmoidoscopy is indicated in patients > 40 with risk factors for colorectal cancer (e.g., weight loss)
Classification of internal hemorrhoids is based on the degree of prolapse
- Grade I: visualized via anoscopy; do not prolapse below the dentate line
- Grade II: prolapse out of the anal canal with defecation or straining but reduce spontaneously
- Grade III: prolapse out of the anal canal with defecation or straining and require manual reduction
- Grade IV: irreducible and may strangulate
Internal hemorrhoids: Stool softeners, sitz baths
- Symptomatic treatment is usually all that is needed: stool softeners (e.g., docusate, psyllium), warm sitz baths (i.e., sitting in a tub of tolerably hot water for 10 min) after each bowel movement, and as needed, anesthetic ointments containing lidocaine, or witch hazel (Hamamelis) compresses.
- Bleeding internal hemorrhoids can be treated by injection sclerotherapy with 5% phenol in vegetable oil. Bleeding should cease at least temporarily.
- Rubber band ligation is used for larger, prolapsing internal hemorrhoids or those that do not respond to conservative management.
Occasionally, excision for thrombosed external hemorrhoids
- Pain caused by a thrombosed external hemorrhoid can be treated with NSAIDs.
- Infrequently, simple excision of the external hemorrhoid is done, which may relieve pain rapidly; after infiltration with 1% lidocaine, the thrombosed portion of the hemorrhoid is excised, and the defect is closed with an absorbable suture.
Question 1 |
proceed with definitive treatment | |
proceed with further investigations Hint: See A for answer | |
prescribe a hemorrhoidal cream Hint: See A for answer | |
do nothing; ask the patient to return in 6 months for review Hint: See A for answer |
Question 2 |
hemorrhoidal cream | |
hemorrhoidal ointment | |
rubber band ligation of the internal hemorrhoids | |
injection of phenol into the hemorrhoidal tissue |
Question 3 |
Internal hemorrhoid | |
External hemorrhoid Hint: significant pain, but no bleeding. | |
Perianal hematoma Hint: Identified by the typical blue tinge under the surface of anal skin | |
Proctitis Hint: No perianal mass. |
Question 4 |
Grade I Hint: bleed only, no prolapse | |
Grade II Hint: prolapsed but reduces spontaneously | |
Grade III Hint: prolapsed and has to be manually reduced. | |
Grade IV |
Question 5 |
Sclerotherapy Hint: appropriate for grade I and II hemorrhoids when conservative measures fail. | |
Hemorrhoidectomy | |
Rubber band ligation Hint: appropriate for grade I and II hemorrhoids when conservative measures fail. | |
Conservative measures Hint: Conservative measures (High fiber diet, increased fluid intake, regular bowel opening) are used in managing grade I hemorrhoids. |
Question 6 |
Ulceration Hint: See C for explanation | |
Portal pyemia Hint: Pyaemia (or pyemia) is a type of septicaemia that leads to widespread abscesses resulting from infected pyaemic thromb. | |
Rectal cancer | |
Anemia Hint: See C for explanation |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture