Patient will present as → a 4-year-old boy is brought to the emergency department by his parents with a sudden onset of high fever, difficulty breathing, and a muffled voice. The parents report that he was fine the previous day but developed symptoms rapidly over the past few hours. They also note that he is drooling and seems to prefer sitting upright, leaning forward. When asked, the parents report, "we don't believe in vaccinations." On examination, the child appears anxious, has a high fever of 39.5°C (103.1°F), and demonstrates significant respiratory distress with stridor. He is drooling and unable to swallow his saliva. His voice is hoarse. A lateral neck X-ray is cautiously performed, revealing a swollen epiglottis, classically described as a "thumbprint" sign, consistent with acute epiglottitis. Due to the risk of airway obstruction, immediate consultation with an otolaryngologist and anesthesiologist is sought for airway management. The child is prepared for potential intubation in a controlled setting. Blood cultures are drawn, and intravenous antibiotics are initiated empirically to cover Haemophilus influenzae type b.
To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
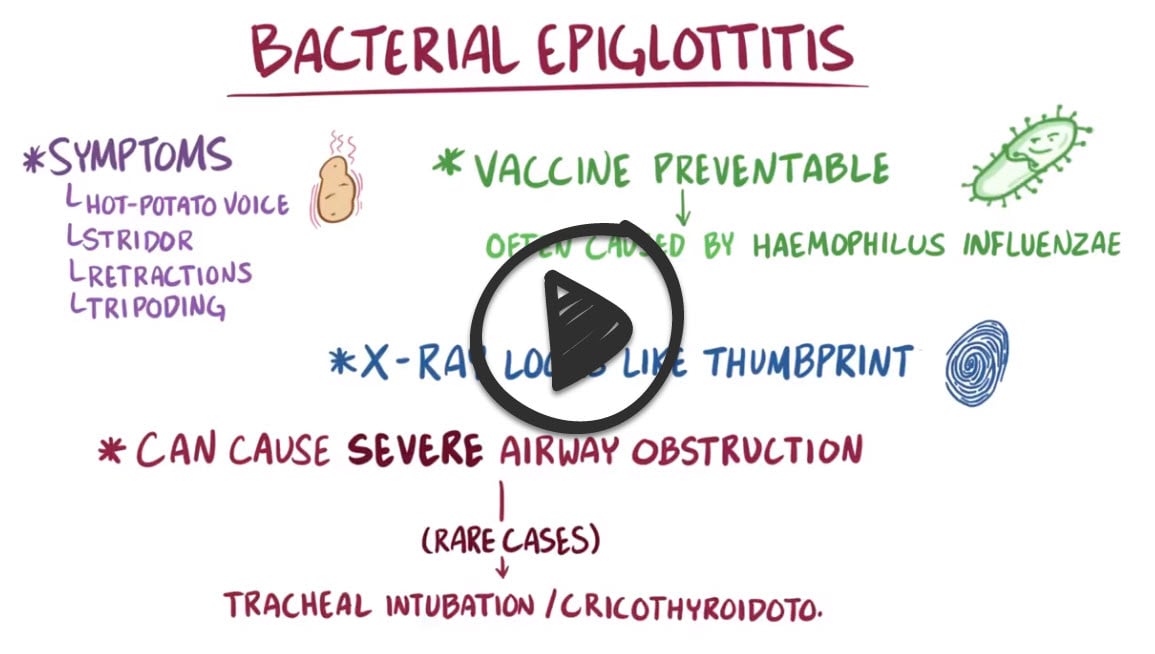
Epiglottitis is supraglottic inflammation/obstruction of the airway due to infection with Haemophilus influenzae
- Considered a medical emergency
- Caused by Haemophilus influenzae Type B bacteria (Hib)
- Hib conjugate vaccine is routinely recommended in a two- or three-dose primary series (at age 2 and 4 months or at age 2, 4, and 6 months, depending upon the vaccine formulation) with a booster dose at age 12 through 15 months
- Underserved areas or nations
- Tripod or "sniffing dog" posture (neck extended)
Signs and symptoms of epiglottitis include inspiratory stridor, restlessness, cough, dyspnea, fever, and drooling
3 D’s of epiglottitis:
- Dysphagia
- Drooling
- Respiratory Distress
Diagnosis of epiglottitis in a person who is stable and breathing comfortably is done with a lateral neck X-ray which will classically show a thumbprint sign from swelling of the epiglottis
- A CT scan would also show a narrow airway from tissue swelling, but lying flat for a CT can obstruct the airway
- Definitive diagnosis is by laryngoscopy (in a controlled clinical setting like the OR)
- The endoscopic appearance of edematous or "cherry red" epiglottis is indicative of epiglottitis
Airway management, first and foremost
- Individuals are often given extra oxygen and in severe cases, may need tracheal intubation
- If tracheal intubation isn’t possible, a needle or surgical cricothyroidotomy may be needed
- Once the airway is stable, antibiotics third-generation cephalosporin (e.g., ceftriaxone or cefotaxime) + an antistaphylococcal agent (e.g., vancomycin or as determined by the local prevalence and sensitivities of MRSA isolates) to treat the infection, and intravenous steroids to decrease the swelling from the immune response
- Immunization against H. influenza type b
- May treat as an outpatient if there is no concern about the airway, otherwise, admit
 Osmosis Osmosis |
|
 |
Epiglottitis is supraglottic inflammation/obstruction of the airway due to infection with Haemophilus influenzae. The Hib vaccine is available to protect against Haemophilus influenzae type b and should be given to infants in three to four divided doses starting at the age of two months. Signs and symptoms of epiglottitis include inspiratory stridor, restlessness, cough, dyspnea, fever, and drooling. It is important to note that the throat should not be examined if epiglottitis is suspected, as this could cause spasm and complete closure of the airway. Assessment of the throat should only be done when immediate endotracheal intubation is possible. Epiglottitis requires emergency treatment.
Play Video + QuizEpiglottitis Interventions
Epiglottitis is supraglottic inflammation/obstruction of the airway due to infection with Haemophilus influenzae. It is important to note that the throat should not be examined if epiglottitis is suspected, as this could cause spasm and complete closure of the airway. Assessment of the throat should only be done when immediate endotracheal intubation is possible. Epiglottitis requires emergency medical treatment.
Haemophilus influenzae
Haemophilus influenzae is a gram-negative coccobacillus that can cause several diseases, including meningitis, pneumonia, otitis media, and epiglottitis. Most strains of H. influenzae live in their host without causing disease, and only cause problems when the host has reduced immune function or inflammation in the area. Naturally acquired disease can occur in infants and young children. Type b Haemophilus influenzae can cause pneumonia and bacterial meningitis. It can also cause otitis media and epiglottitis. In fact, this organism is the most common etiologic agent associated with epiglottitis, which has a thumbprint sign seen on X-ray. Ceftriaxone antibiotic is commonly used for treatment in severe cases.
Play Video + QuizQuestion 1 |
Croupy cough and drooling | |
Thick gray, adherent exudate Hint: Thick gray adherent exudate is suggestive of diphtheria. | |
Beefy red uvula, palatal petechiae, white exudate Hint: Beefy red uvula, palatal petechiae, and white exudate are findings suggestive of streptococcal pharyngitis. | |
Inflammation and medial protrusion of one tonsil Hint: Inflammation with medial protrusion of the tonsil is suggestive of a peritonsillar abscess. |
Question 2 |
Rhinovirus Hint: Causes upper respiratory infections but not a common cause of epiglottitis. | |
Streptococcus pneumoniae Hint: Can infect the respiratory tract but not a prime cause of epiglottitis. | |
Neisseria meningitidis Hint: Associated with meningitis more than epiglottitis. | |
Haemophilus influenzae type B | |
Group A Streptococcus Hint: Leads to pharyngitis and tonsillitis more often than epiglottitis. |
Question 3 |
Throat culture Hint: Difficult to obtain and does not provide specific information in this case. | |
Lateral neck X-ray | |
Complete blood count Hint: Not specific for diagnosing epiglottitis. | |
Monospot test Hint: Checks for EBV infection unrelated to this child's presentation. | |
Rapid streptococcal test Hint: Useful for pharyngitis but not epiglottitis. |
Question 4 |
Intravenous antibiotics Hint: Treat the underlying infection but do not address the airway obstruction. | |
Nebulized racemic epinephrine Hint: May transiently improve stridor but intubation is still required. | |
Intubation | |
Oral corticosteroids Hint: Do not improve the airway obstruction requiring intubation | |
Cool mist humidification Hint: May provide some symptomatic relief but does not address need for intubation. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture




