Patient will present as → a 65-year-old man comes to the office due to 3 days of progressive dyspnea and purulent sputum production. The patient takes albuterol and tiotropium bromide for moderate chronic obstructive pulmonary disease. His medical history is relevant for a 40-pack-year smoking history, type II diabetes mellitus, hyperlipidemia, and coronary artery stenting 2 years ago. Physical exam shows a barrel-shaped chest, inspiratory crackles, hepatojugular reflux, pulsus paradoxus, and ventricular gallop. His temperature is 38.1°C (100.5°F), the pulse is 130/min, respirations are 28/min, blood pressure is 130/84 mmHg, and pulse oximetry on room air shows an oxygen saturation of 86%.
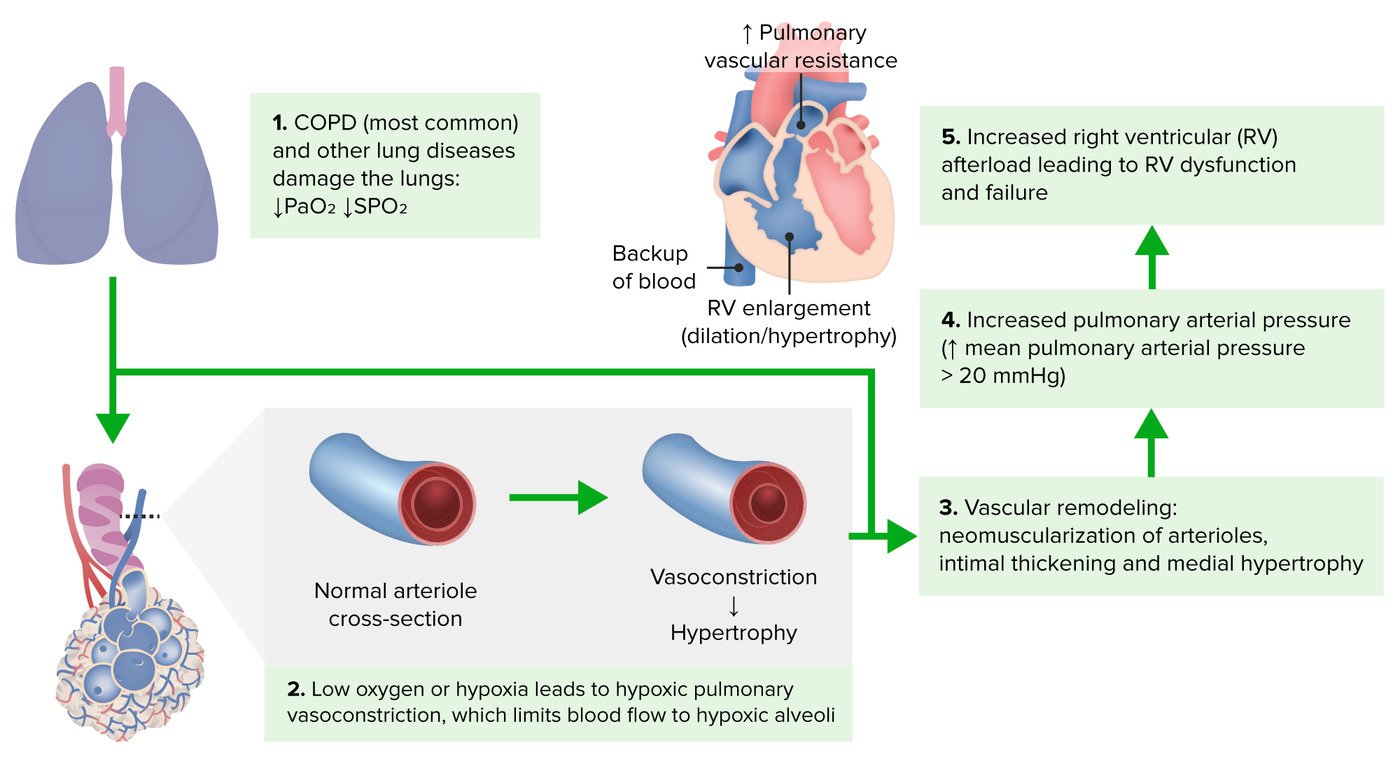
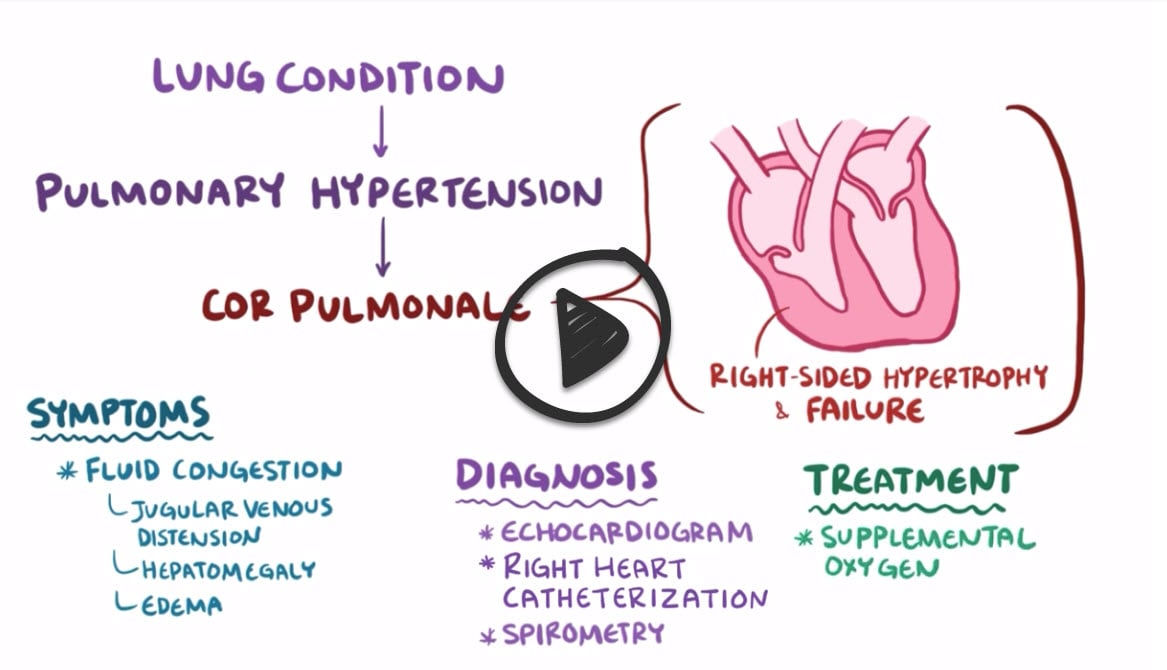
Cor pulmonale is right ventricular enlargement and eventually failure secondary to a lung disorder that causes pulmonary artery hypertension
- Lung disorders such as PE, vasculitis, ARDS, COPD (most common), asthma, and ILD cause pulmonary artery hypertension
- Pulmonary artery hypertension then leads to right ventricular failure
- Findings include peripheral edema, neck vein distention, hepatomegaly, and a parasternal lift
The diagnosis of cor pulmonale is usually made with an echocardiogram → increased pressure in the pulmonary arteries and right ventricle
- Spirometry can be done to look for chronic lung disease
- The gold standard diagnostic test to directly measure pulmonary pressures and assess for response to vasodilating medications is a right heart catheterization
Treatment of chronic cor pulmonale generally focuses on the underlying pulmonary disease
- Early identification and treatment of the cause are important before cardiac structural changes become irreversible
- Although patients may have significant peripheral edema, diuretics are not helpful and may be harmful; small decreases in preload often worsen cor pulmonale
- Right ventricular ischemia or pulmonary artery stretching can cause anginal chest pain in cor pulmonale that does not respond to nitrates
Question 1 |
cor pulmonale | |
chronic bronchitis | |
emphysema | |
pneumonia |
Question 2 |
acute coronary syndrome Hint: Marked hypotension in acute coronary syndrome occurs when the right coronary artery is affected. Acute coronary syndromes do not usually present with systolic murmurs, but patients will complain of angina and the ECG changes will include ST-segment changes. | |
cor pulmonale | |
heart failure Hint: Patients who have severe heart failure will have similar symptoms but also have pulsus alternans and pulmonary rales. | |
pulmonary embolus Hint: patients with pulmonary embolus may have hemodynamic changes but usually have a low PaO2 and a normal PaCO2. ECG may show right-axis deviation in a pulmonary embolus as well. |
|
List |
References: Merck Manual · UpToDate


 Osmosis
Osmosis