Patient with Histoplasmosis will present with → a 21-year-old male presents with a cough and mild shortness of breath for three days. The cough is productive of yellowish mucus. He reports a low-grade fever with this episode but says that he has otherwise been healthy. He has spent the last month working in bat caves. He denies tobacco or alcohol use.
Patient with valley fever will present as → a 38-year-old construction worker who recently moved to Phoenix, Arizona, for a new project. Over the past two weeks, he's been experiencing fatigue, cough, and intermittent fevers. He also mentions having chest pain that worsens when he takes a deep breath. He recalls a dusty wind storm at the construction site about three weeks ago. On physical examination, you note a few erythematous, tender nodules on his shins. Chest radiography shows a nodular pattern in the right lung field. Given his symptoms and exposure history, a sputum sample is sent for fungal cultures.
Patient with Pulmonary aspergillosis will present as → a 55-year-old man with a history of chronic obstructive pulmonary disease (COPD) and recent influenza infection presents to the emergency department with a 2-week history of worsening cough, hemoptysis, and shortness of breath. He has lost 5 kg over the past month and reports night sweats. His temperature is 38.3°C (101°F), heart rate is 102 beats per minute, and respiratory rate is 28 breaths per minute. Chest X-ray reveals a cavitary lesion in the upper lobe of the right lung.
Patient with Cryptococcus will present as → a 49-year-old HIV-positive male with a CD4 count of 9. He lives alone and drinks daily. He presents to the hospital with a headache, neck stiffness, and confusion. A lumbar puncture (LP) shows that his intracranial pressure is very high (45 cm) and that his spinal fluid contains Cryptococcus (India Ink and CrAg positive). Baseline blood ordered: full blood count, creatinine, ALT, and RPR. The serum cryptococcal antigen (CrAg) test is positive.
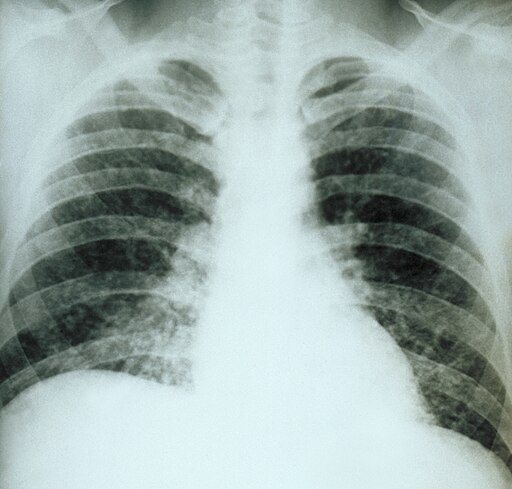
Patient with PJP Pneumonia will present as → a 32-year-old man with a two-week history of fever and dry, nonproductive cough. For the past five days, he has been having shortness of breath. There is no history of pleuritic chest pain or rigors.Past medical history is significant for HIV. His temperature is 100.4°F (38°C), pulse is 92/min, O2 saturation is 92%, respirations are 18/min, and blood pressure is 120/70 mmHg. Purified protein derivative (PPD) is negative. CD4 cell count is 190. The chest exam reveals bibasal crackles. The chest radiograph shows interstitial infiltrates bilaterally. The patient's condition worsens on levofloxacin.
Fungal pneumonia is common in immunocompromised patients – AIDS, steroid use, organ transplant
1. Coccidioides (valley fever): Look for this in a patient with non-remitting cough/bronchitis non-responsive to conventional treatments
- Caused by fungal inhalation in western states
- Serologic tests using enzyme-linked immunoassays (EIA) for IgM and IgG should be ordered first, if possible. If the EIA is positive, a confirmatory immunodiffusion test should be performed
- Treatment: fluconazole or itraconazole.
2. Pulmonary aspergillosis: The majority of cases occur in people with underlying illnesses such as tuberculosis or chronic obstructive pulmonary disease (COPD) but with otherwise healthy immune systems
- Treatment: fluconazole or itraconazole
3. Cryptococcus: found in soil, can disseminate and can cause meningitis
- Immunocompromised patients are usually symptomatic
- Lumbar puncture for meningitis
- Treatment: Amphotericin B
4. Histoplasma capsulatum: Chronic cavitary histoplasmosis is characterized by pulmonary lesions that are often apical and resemble cavitary TB. Manifestations are worsening cough and dyspnea, progressing eventually to disabling respiratory dysfunction. Dissemination does not occur.
- Bird or bat droppings (caves, zoo, bird)
- Mississippi or Ohio river valley
- Mediastinal or hilar lymphadenopathy (looks like sarcoid)
- Treatment: Amphotericin B
5. Pneumocystis Jiroveci: Formerly PCP Pneumonia now called (PJP) (there are other HIV-related pneumonias but this is the one you will need to know for the test)
- Common in HIV-infected patients with a low CD4 count of less than 200
- The radiograph shows diffuse interstitial or bilateral perihilar infiltrates
- Diagnose with bronchoalveolar lavage (PCR), labs, and an HIV test
- Treat with Trimethoprim-sulfamethoxazole (BACTRIM) and steroids
- Prophylaxis for high-risk patients with a CD4 count of less than 200 or with a history of PJP infection. Daily Bactrim is the prophylaxis antibiotic of choice
Chest X-Ray Findings:
- Cryptococcus: Cryptococcal antigen can be detected in CSF and serum. India ink stain or serology with latex agglutination assay or cryptococcal antigen assay (CRAG) is helpful.
- Histoplasma capsulatum causes mediastinal or hilar lymphadenopathy (looks like sarcoidosis)
- Pneumocystis Jiroveci
- Diagnose with bronchoalveolar lavage (PCR), labs, and an HIV test
- causes diffuse interstitial or bilateral perihilar infiltrates
Cryptococcus and Histoplasma - Amphotericin B
Coccidioides - Azoles - fluconazole or itraconazole
Aspergillus - Triazoles - Triazole antifungal agents include voriconazole, posaconazole, itraconazole, and fluconazole
Coccidioidomycosis is a systemic fungal disease caused by Coccidioides immitis, a dimorphic fungus that exists as a mold in cool temperatures and spherules in warm temperatures like soft tissue. The fungus is found as a mold in the soil, and produces hyphae with arthrospores that are easily dispersed throughout the air and inhaled. When the arthrospores are inhaled, they form spherules filled with endospores. These spherules measure 20-60 um and contain endospores that are slightly larger than red blood cells, which are around 6-8um. The spherules rupture and endospores spread throughout the body causing disease, most commonly in the lung, skin, bone, and brain. Most frequently, coccidiomycosis causes pneumonia, but it can also disseminate and cause meningitis or osteomyelitis. Common skin findings include erythema nodosum, which are painful red nodules found on the extensor surfaces like the anterior lower legs. Coccidioidomycosis typically causes granulomatous inflammation with caseous necrosis, which is a type of white cheesy appearing necrosis. C.immitis is commonly found in the Southwestern United States, particularly the San Joaquin valley region, in deserts and in construction zones where the spores can be carried by dust storms. Any disruption of the soil can increase spread of the organism; thus, coccidioidomycosis infections are also more frequent after earthquakes. No treatment is required for asymptomatic infections, but azoles can be used for systemic infections.
Play Video + QuizAspergillus
Aspergillus is a genus of monomorphic fungi named after the shape of an aspergillum, which is an instrument used to sprinkle holy water. Aspergillus fumigatus is one of the most common Aspergillus species to cause disease. Its spores are ubiquitous in the atmosphere and estimated that everybody inhales several hundred spores daily. The most common forms of disease are allergic bronchopulmonary aspergillosis, pulmonary aspergilloma, and invasive aspergillosis. On microscopy, Aspergillus can be identified by their septate hyphae that tend to have dichotomous branches at primarily acute angles of about 45 degrees. The organisms can also demonstrate fruiting bodies which are the conidial heads that produce spores. Allergic bronchopulmonary aspergillosis is associated with hypersensitivity to the spores of Aspergillus molds, commonly seen in asthmatics. It is characterized by numerous eosinophils and elevated IgE directed against aspergillus antigens. Thick mucus plugs can develop and overtime cause the bronchi to become dilated leading to bronchiectasis. Aspergilloma refers to growth of the fungus within a cavity of the lung, previously formed during an illness such as tuberculosis. The spores penetrate the cavity and germinate, causing the formation of a fungal ball within the cavity. Within the cavity, the fungus secretes toxic and allergic products. Hemoptysis is common, occurring in 50-80% of affected individuals. Invasive aspergillosis occurs in immunocompromised individuals including people with chronic granulomatous disease where the fungus transfers from the lungs to the bloodstream and can disseminate to the brain or other organs. Within the blood vessels, the organism can cause hemorrhagic infarctions and cause necrotizing bronchopneumonia in the lungs.
Cryptococcus neoformans
Cryptococcus neoformans is an opportunistic fungal infection that causes cryptococcosis, a severe disease of the CNS. C. neoformans is monomorphic and only exists as yeast with narrow-based buds measuring 5-10 um. It is encapsulated with a polysaccharide capsule that helps evade phagocytosis. In addition, its virulence is increased by the ability to undergo phenotypic switching and change the structure of its capsule. It is commonly found in the soil or in pigeon droppings and can cause disease when inhaled. Healthy individuals can demonstrate a range of symptoms, from asymptomatic to pneumonia or meningoencephalitis. However, immunosuppressed patients, such as HIV/AIDS patients or patients on chronic corticosteroid therapy, are most commonly affected and more likely to have disseminated disease. Dissemination into the CSF can commonly cause meningitis that extends into the perivascular space with lesions that appear similar to soap bubbles. Diagnosis of cryptococcosis can be made in many different ways. A Gram stain of the organism collected from CSF stained with India ink reveals the oval yeast with a halo surrounding it, signifying the capsule. A mucicarmine stain or periodic acid-Schiff stain can also be used, which stains the polysaccharide capsule a bright red. In addition, a latex agglutination test can also be used, which uses antibody-coated latex beads that binds to cryptococcal antigen present in the assay. Treatment includes amphotericin B and flucytosine for meningitis and disseminated disease. Fluconazole can also be used as long-term prophylaxis in immunosuppressed patients
Play Video + QuizHistoplasma
Histoplasma is a genus of dimorphic fungi known to be the causative agent of histoplasmosis. This organism has a yeast form that is 2-5 um and found within macrophages within the body. It is commonly found in bat and Starling bird feces and contracted by inhalation of the spores. Therefore, it is commonly associated with entrance into caves and is most prevalent in the Ohio and Mississippi river valleys. Symptoms of this infection vary but the disease primarily affects the lungs, causing pneumonia. Occasionally, the organism can disseminate and affect other organs including the meninges, liver, or adrenals and widely disseminated disease can occur in the immunocompromised. Histoplasma infections produce granulomas, which usually undergo caseation necrosis and can form large areas of consolidation. Like most systemic mycoses, treatment includes an azole antifungal for local infection along with amphotericin B for systemic infection.
Play Video + QuizPneumocystis jiroveci
Pneumocystis jiroveci is a fungal infection which typically presents with hypoxia and fever in the lungs of immunocompromised patients. The infection is usually diagnosed using classic x-ray findings of diffuse interstitial infiltration bilaterally. Definitive diagnosis can be made using lavage or biopsy, were it can be identified by methenamine on silver stain. In order to prevent the disease in patients with HIV and CD4 counts below 200, TMP-SMX is used prophylactically. TMP-SMX is also used as treatment for diagnosed disease.
Play Video + QuizAmphotericin B
Amphotericin B is a polyene medication, which works by binding to ergosterol in fungal cell membranes. It forms membrane pores, causing electrolytes to leak, killing the fungal cell. It is used for serious, systemic mycoses. It can lead to the side effects of fever and chills, nephrotoxicity, arrhythmias, anemia and IV phlebitis.
Play Video + QuizAmphotericin B Side Effects & Toxicity
Amphotericin B is a polyene medication, which works by binding to ergosterol in fungal cell membranes. It forms membrane pores, causing electrolytes to leak, killing the fungal cell. It is used for serious, systemic mycoses. It can lead to the side effects of fever and chills, nephrotoxicity, hypotension, arrhythmias, anemia and IV phlebitis.<br />
Play Video + QuizQuestion 1 |
cryptococcosis Hint: Cryptococcus is most likely in people exposed to pigeons and is also found in soil enriched by bird droppings or in cockroach-infested environments. | |
histoplasmosis | |
psittacosis Hint: Parrots, parakeets, ducks, and turkeys are the usual hosts and most commonly infected species for psittacoccal infections as well. It is less common in humans. | |
Candidal species |
Question 2 |
Ceftriaxone | |
Tetracyline | |
Ciprofloxacin | |
Mefloquin | |
Fluconazole |
Question 3 |
Amphotericin B and flucytosine | |
Metronidazole | |
Acyclovir | |
Amantadine | |
Penicillin G |
|
List |
References: Merck Manual · UpToDate


 Picmonic
Picmonic