8-year-old with 3 months of cough, night sweats, and arthritis
Patient will present as → a 78-year-old man with a 3-month history of weight loss, fever, fatigue, night sweats, and cough. He is a former smoker. A recent HIV test was negative. A chest CT reveals a 3 cm lesion in the upper lobe of the left lung and calcification around the left lung hilus. A sputum smear was positive for acid-fast organisms.
Organism: Mycobacterium tuberculosis: transmitted by respiratory droplets
- Classic findings include fever, night sweats, anorexia, and weight loss
There are two kinds of tests that are used to detect TB bacteria in the body: the TB skin test (TST) and TB blood tests (IGRAs)
- A positive TST or IGRA only tells that a person has been infected with TB bacteria. It does not tell whether the person has latent TB infection (LTBI) or has progressed to TB disease
- IGRAs are the preferred method of TB testing for people who have received the BCG vaccine and those who may have a difficult time returning for a second appointment to have a TST read
- The TB skin test is the preferred TB test for children under the age of five
PPD Rules:
PPD Skin Test Interpretation Based on CDC Guidelines – Area of induration = raised area (not the red area)
The result of the PPD test is either positive or negative. However, the size of the induration diameter cutoff (5, 10, or 15 mm) for the test to be considered positive is based on certain risk factors.
< 5 mm: Induration of less than 5 mm is considered positive in the following cases:
- Individuals infected with HIV who have had close contact with an active contagious case
≥ 5 mm: Induration of 5 mm or greater is considered positive in the following cases:
- Immunosuppressed individuals, including those receiving long-term steroids (the equivalent of prednisone ≥15 mg/day for ≥1 month), chemotherapy, or tumor necrosis factor-alpha inhibitors
- Individuals infected with HIV
- Close contact with patients with active TB
- Prior TB signs on chest radiography, such as fibronodular changes
- Organ transplant recipients
≥ 10 mm: Induration of 10 mm or more is considered positive in the following cases:
- Emigrants from countries where TB is considered endemic or the incidence of infection is greater than 25/100,000
- Employees and residents in high-risk settings, such as prisons, mycobacteriology labs, healthcare settings, and homeless shelters
- Injection drug users
- Mycobacteriology laboratory professionals
- Children less than four years of age
- Those with chronic medical conditions that increase the risk of reactivation TB, including diabetes mellitus, chronic renal failure on dialysis, silicosis, malignancy (leukemia, lymphoma, or cancer of the head, neck, or lung), a history of jejunoileal bypass
- Individuals weighing less than 90% of the ideal body weight
- Infants, children, and adolescents exposed to those in high-risk categories
≥ 15 mm: Induration of 15 mm or more is considered positive in the following cases:
- Healthy individuals older than four years of age with a low likelihood of TB infection
Who should be tested for latent tuberculosis infection (LTBI)?
| Individuals with an increased risk of new TB infection |
| Close contacts of patients with untreated active respiratory TB |
| Casual contacts of patients with untreated active respiratory TB |
| People who use illicit drugs |
| Residents or employees of a homeless shelter or correctional facility |
| Health care workers (HCWs) in some circumstances |
| Individuals with an increased risk of reactivation |
| High risk (test all patients) |
| HIV infection (any stage of illness) |
| Transplant, chemotherapy, or other major immunocompromising condition |
| Lymphoma, leukemia, head and neck cancer |
| Abnormal chest radiograph with apical fibronodular changes typical of healed TB (not including granuloma) |
| Silicosis |
| Renal failure (requiring dialysis) |
| Treatment with TNF-alpha inhibitors |
| Moderate risk (test patients in groups with increased prevalence of LTBI) |
| Diabetes mellitus |
| Systemic glucocorticoids (≥15 mg/day for ≥1 month) |
| Slightly increased risk (test patients in groups with increased prevalence of LTBI) |
| Underweight (<85 percent of ideal body weight); for most individuals, this is equivalent to body mass index (BMI) ≤20 |
| Cigarette smoker (≥1 pack/day) |
| Chest radiograph with solitary granuloma |
| Individuals born in or former residents of countries with high incidence of TB disease (WITHOUT other risk factors listed above) |
All persons with either symptoms or a positive TB test (TST or IGRA) result should be evaluated for TB disease. If a person has symptoms, but a negative TB test result, they should still be evaluated for TB disease
Diagnose TB with sputum for AFB smears and cultures
- Isolate hospitalized patients who may have TB (cough for 3 weeks, night sweats, hemoptysis, etc.) and send three sputum specimens for acid-fast bacilli staining (AFB smears) and Mycobacterium tuberculosis cultures
Xray: upper cavitary lesions, infiltrates, and ghon complexes in the apex of lungs
- Ghon complex (calcified lymph + lesions)
- Biopsy: Caseating granulomas
Miliary Tb (Tb spread outside the lungs)
- Potts DZ - Tb to spine
- Scrofula - Tb to cervical lymph nodes
If PPD/IGRA is + order a CXR
- If CXR negative - Latent TB treat for latent TB (see below)
- Pt's on INH should take supplemental Vitamin B6 (pyridoxine) daily to prevent neuropathy
CDC recommends short-course, rifamycin-based, 3- or 4-month latent TB infection treatment regimens over 6- or 9-month isoniazid monotherapy. Short course regimens include:
- Three months of once-weekly isoniazid plus rifapentine (3HP)
- Four months of daily rifampin (4R)
- Three months of daily isoniazid plus rifampin (3HR)
Active treatment:
Several treatment regimens are recommended in the United States for active TB disease. TB treatment can take 4, 6, or 9 months depending on the regimen.
- 4-month Rifapentine–moxifloxacin TB treatment regimen
- High-dose daily rifapentine (RPT) with
- Moxifloxacin (MOX): QT-prolonging agent and has been associated with cardiac arrhythmias, which may be fatal
- Isoniazid (INH) and
- Pyrazinamide (PZA)
The 4-month rifapentine-moxifloxacin regimen has an intensive phase of 2 months, followed by a continuation phase of 2 months and 1 week (total 17 weeks for treatment).
- 6- or 9-month quad therapy (RIPE) TB treatment regimen: Rifampin, Isoniazid, Pyrazinamide, Ethambutol
- Rifampin (RIF): Orange body fluids, hepatitis – “remember R = red/orange body fluids”
- Isoniazid (INH): Peripheral neuropathy (given with B6- pyridoxine 25 to 50 mg/day)
- Pyrazinamide (PZA): Hyperuricemia (Gout)
- Ethambutol (EMB): Optic neuritis, red-green blindness – “remember E = eyes”
All are hepatotoxic, so you need to get baseline labs
- Hepatitis attributed to antituberculous drugs should prompt discontinuation of all hepatotoxic drugs if the serum bilirubin is ≥3 mg/dL or serum transaminases are more than five times the upper limit of normal!
" Did you know that patients need to be tested for tuberculosis prior to being treated with etanercept (Enbrel). Etanercept is an anti-cytokine agent used in the treatment of rheumatoid arthritis and has as a side effect the potential for serious infections. One of these side effects includes the reactivation of dormant tuberculosis."
Most outpatients will be managed by your local health department to directly observe them taking TB meds, for monitoring, etc.
- Patients with active TB will need two negative AFB smears and cultures in a row for therapy cessation
- Prophylaxis for household members may be considered
Treatment Summary
- We know to isolate hospitalized patients who may have TB (cough for 3 weeks, night sweats, hemoptysis, etc)...and send three sputum specimens for acid-fast bacilli and Mycobacterium tuberculosis cultures.
- Order a newer nucleic acid amplification tests. It is better at identifying TB versus other forms of Mycobacterium...can help detect possible TB sooner...and help get patients out of isolation earlier.
- Start empiric treatment in those likely to have TB...such as a symptomatic patient with TB exposure. Use culture results to confirm the diagnosis...these are usually available within 6 weeks.
- Treat with multiple drugs for several months.
- Monitor serum creatinine and adjust dosing, if needed. For example, reduce ethambutol and pyrazinamide dosing to three times per week instead of daily in patients with a CrCl of less than 30 mL/min.
- Add pyridoxine 25 to 50 mg/day when isoniazid is used in patients at risk for neuropathy...such as those with alcoholism, diabetes, or HIV.
- Most outpatients will be managed by your local health department...to directly observe them taking TB meds, for monitoring, etc.
- Reinforce ways to improve med efficacy in your office...such as advising to take most TB meds on an empty stomach since food can reduce absorption. If patients complain of nausea, try adding an antacid.
- Watch for hepatotoxicity with isoniazid, pyrazinamide, or rifampin...and severe side effects such as rash, drug fever, etc.
- Also, be aware of drug interactions...especially with HIV meds. For example, double the raltegravir (Isentress) dose when used with rifampin.
*Please refer to the treatment tab for the most up-to-date treatment guidelines
 Osmosis Osmosis |
|
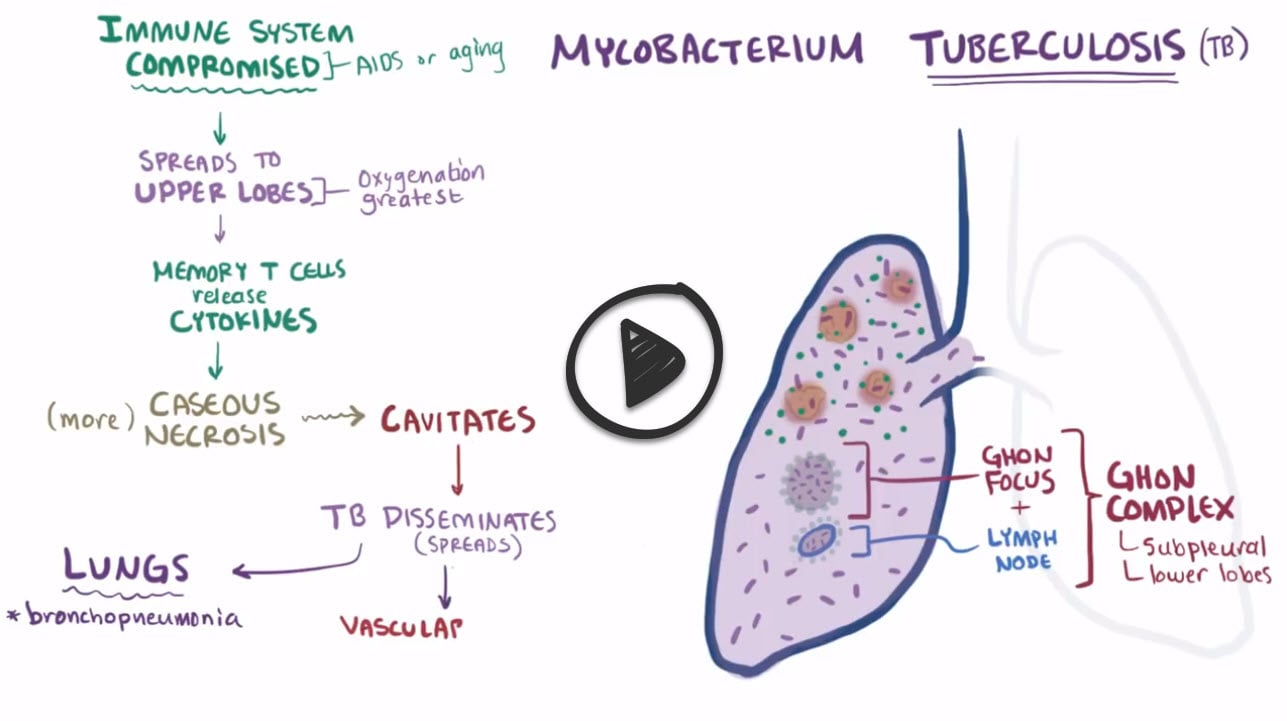 |
Tuberculosis is caused by Mycobacterium tuberculosis and is the leading cause of death worldwide from an infectious bacterial disease. Mycobacterium are noted for having mycolic acid cell walls, which make them acid fast and stain to carbolfuchsin red. Cell smears from colonies have a distinctive look that resembles serpentine cords. Primary tuberculosis is the form of disease that occurs in a previously unexposed person. Most people do not develop clinically significant disease. The inhaled bacillus implants in the lower part of the upper lobe and can cause a focus of inflammation and consolidation called a ghon focus. The bacilli can drain to regional lymph nodes and the combination of a ghon focus with perihilar lobar lymph nodes constitutes a ghon complex. Secondary tuberculosis occurs in previously exposed people via reactivation of a latent infection but can also occur from a new exposure in the immunocompromised. Secondary pulmonary tuberculosis typically involves the apex of the upper lobes because the upper regions of the lungs are well-aerated where the bacteria thrive. Systemic symptoms commonly include fever, weight loss and night sweats. Many patients also present with hemoptysis. Tuberculosis can spread beyond the lungs when the bacteria disseminate through the systemic arterial system. Common organs involved include the adrenal glands, CNS, GI, liver, vertebrate, kidneys, and bone.
Play Video + QuizTuberculosis Skin Mantoux Test (PPD)
A Mantoux test using purified protein derivative (PPD) is performed as a standard screening test for tuberculosis (TB). Memory cells generated during the body’s initial cell-mediated response to TB will react to the PPD intradermal injection, creating a delayed hypersensitivity reaction and a positive TB skin test. The results of the skin test must be interpreted by a nurse within 48 to 72 hours of receiving the PPD injection and are invalid when read before or after the allotted time frame. A positive test result will appear as an induration or a hardened mass, which is then measured to determine if the patient has tested positive or negative. Patients who test positive for TB should also get a chest x-ray to confirm or substantiate the diagnosis.
Ethambutol
Ethambutol is a bacteriostatic antimycobacterial drug used in the treatment of tuberculosis. It is often given in combination with isoniazid, rifampin, and pyrazinamide for treatment of active TB. This drug works by blocking bacterial arabinosyl transferase enzyme, which polymerizes carbohydrates in the bacterial cell wall. Disruption of this bacterial enzyme therefore leads to increased permeability of the cell wall. This drug can be especially toxic to the eyes, with adverse effects of optic neuritis and red-green color blindness reported.
Play Video + QuizIsoniazid
Isoniazid is a drug used in the treatment of both latent and active tuberculosis. It can be used as a monotherapy for the treatment of latent tuberculosis but is commonly used in a four-drug regimen including pyrazinamide, ethambutol, rifampin for active TB. Isoniazid is a pro-drug and requires bacterial catalase-peroxidase enzyme to activate it and works by inhibiting the synthesis of mycolic acid. It is metabolized in the liver via acetylation. There are two forms of the acetylating enzyme, a fast acetylator and a slow acetylator. Those with the fast acetylator metabolize the drug more quickly than the slow acetylators. Common side effects include vitamin B6 deficiency, hepatotoxicity and neurotoxicity. Isoniazid is also associated with drug induced lupus erythematosus.
Play Video + QuizRifampin
Rifampin, also called rifampicin, is a bactericidal antibiotic commonly used in the treatment of active tuberculosis. Rifampin inhibits bacterial RNA synthesis by inhibiting RNA polymerase. Rifampin resistance can develop quickly due to alteration of the binding sites on RNA polymerase so monotherapy should not be used in treatment of infections. Instead, rifampin is commonly used in combination with other antibiotics. Besides mycobacterium TB, rifampin is also used in the treatment of haemophilus influenza, leprosy, and meningitis. Rifampin is a well known P450 inducer and can increase the rate of metabolism of other drugs that are cleared by the liver through the p450 system. Taking rifampin can cause bodily fluids like urine and tears to become orange red in color, which may be alarming but is completely benign.
Play Video + QuizQuestion 1 |
positive | |
negative Hint: See A for explanation. | |
active infection Hint: A positive PPD identifies patients that have been infected with Mycobacterium tuberculosis, but does not indicate whether the disease is currently active or inactive. | |
falsely negative Hint: See A for explanation. |
Question 2 |
A child with cystic fibrosis Hint: Children with cystic fibrosis are at an increased risk for various lung infections, but not drug resistance. | |
An elderly patient in a nursing home Hint: While institutionalized patients, such as nursing home residents, are at increased risk for infection with Mycobacterium tuberculosis, the patient is not at increased risk for drug resistance. | |
Non-adherence to prescribed drug regimen | |
Patients with a history of diabetes mellitus Hint: Patients with a history of diabetes mellitus are at increased risk for active disease, not drug resistance. |
Question 3 |
etanercept (Enbrel).
| |
cyclosporine (Neoral). Hint: Cyclosporine, methotrexate, and prednisone do not have the requirement to check for tuberculosis prior to initiating treatment. | |
methotrexate (Rheumatrex). Hint: See B for explanation. | |
prednisone (Deltasone). Hint: See B for explanation. |
Question 4 |
Hyperinflation and flat diaphragms Hint: Chest x-ray findings of hyperinflation and flat diaphragms suggest long-standing chronic obstructive lung disease. | |
Interstitial fibrosis and pleural thickening Hint: Interstitial fibrosis and pleural thickening on a chest x-ray are found in cases of interstitial lung disease. | |
Cavitary lesions involving the upper lobes | |
"Eggshell" calcification of hilar lymph nodes Hint: Chest x-ray findings of "eggshell" calcification of hilar lymph nodes strongly supports a diagnosis of silicosis. |
Question 5 |
Four-drug regimen for 4 months Hint: Greater than 5 mm of induration is positive in an HIV-infected patient. A positive PPD and negative chest film is considered latent TB infection and, while requiring treatment, does not require the full four-drug regimen. | |
Isoniazid with Rifampin | |
Observation only Hint: Latent TB infection is associated with a risk of progression to tuberculosis and observation alone is inadequate. | |
Repeat PPD and chest radiograph in 3 months Hint: Repeat screening is not helpful since the diagnosis of latent TB infection has already been established. |
Question 6 |
Sputum induction Hint: Sputum induction should not be used as a screening test for tuberculosis. | |
PPD skin test Hint: See E for explanation | |
Chest x-ray Hint: A chest X-Ray will need to be performed if this patient's initial screening is positive. In this case >10 mm TST or a + IGRA | |
No screening needed Hint: This patient has recently emigrated from a possible endemic region and should be screened for tuberculosis. | |
TB blood test (IGRA) |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture