Patient will present with → a 6-month-old boy brought to the clinic by his mother, who is worried about his persistent and severe coughing episodes that have been ongoing for two weeks. She describes the cough as initially mild but has since progressed to intense bouts followed by a high-pitched "whooping" sound when he takes a breath. These episodes often lead to vomiting and have been particularly distressing at night. The mother also mentions that her son had a mild fever and runny nose before the cough started. On examination, the infant has clear lung sounds between coughing fits, but during an episode, inspiratory whoops can be heard. A nasopharyngeal swab is taken for further testing. (watch video)
Patient will present as → a 24-year-old with an increasing cough for 3 weeks. The cough comes and goes, sometimes lasting for 10 minutes and causing gasping inhalations. The cough was preceded by a mild cough and cold 2 weeks ago. She has no known drug allergies. The patient's immunizations are not up-to-date. (alternate presentation)
Caused by the highly contagious gram-negative bacteria Bordetella Pertussis
- Consider pertussis in adults with cough > 2 weeks
- Unvaccinated or individuals whose vaccinations are not up-to-date
- Symptoms are initially those of nonspecific upper respiratory infection (catarrhal stage ) followed by paroxysmal or spasmodic coughing that usually ends in a prolonged, high-pitched, crowing inspiration (the whoop)
Diagnosis is confirmed by nasopharyngeal secretions
- In the setting of a pertussis outbreak or known close contact with a confirmed case, the presence of a cough lasting ≥ 2 weeks is sufficient for clinical diagnosis (even in the absence of other symptoms)
- For patients with less than two weeks of cough in whom there is a clinical concern for pertussis, perform both culture and PCR for B. pertussis
- For patients with two to four weeks of cough, perform both culture and PCR
- For patients with more than four weeks of cough, only serology is useful
Treat with macrolide antibiotic erythromycin or azithromycin
- Trimethoprim/sulfamethoxazole may be substituted in patients ≥ 2 months who are intolerant of or hypersensitive to macrolide antibiotics
- Supportive care with steroids and/or beta2 agonists
"What do you do if your patient is a 4-year-old diagnosed with pertussis and attends a daycare? All close contacts of a patient with pertussis should be treated with macrolide prophylaxis regardless of age, immunization history, or symptoms."
Postexposure Antimicrobial Prophylaxis CDC Guidelines
Children should get 5 doses of DTaP vaccine: one dose at each of the following ages:
- 2 months
- 4 months
- 6 months
- 15–18 months
- 4–6 years
Adolescents 11 through 18 years of age (preferably at age 11-12 years) should receive a single booster dose of Tdap
- One dose of Tdap is also recommended for adults 19 years of age and older who did not get Tdap as an adolescent
- Expectant mothers should receive Tdap during each pregnancy, preferably at 27 through 36 weeks
- Tdap should also be given to 7-10-year-olds who are not fully immunized against pertussis
- Tdap can be given no matter when Td was last received
 Osmosis Osmosis |
|
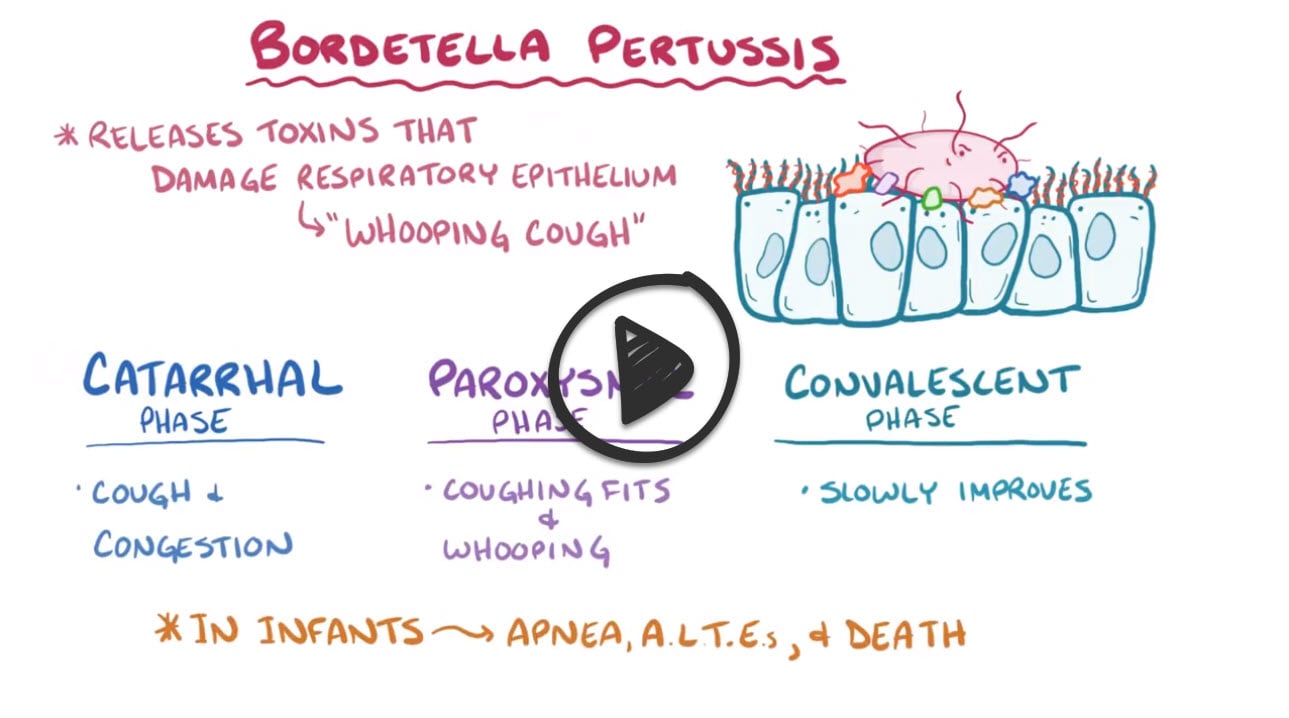 |
Bordetella pertussis is a gram-negative coccobacillus that is the causative agent of whooping cough. This organism is typically cultured on specialized medium called Bordet Gengou agar. Bordetella pertussis produces the pertussis toxin, which is an ADP ribosylating AB toxin that is involved in the colonization of the respiratory tract and the establishment of infection. This toxin catalyzes the ADP ribosylation of the Gi subunit, which prevents the G proteins from interacting with G protein coupled receptors on the cell membrane. The Gi subunits remain locked in an inactive or off state and are therefore unable to inhibit adenylyl cyclase activity leading to increased concentrations of cAMP. The increase in intracellular cAMP has several systemic effects including lymphocytosis and an increase in insulin leading to hypoglycemia.
The first 1-2 weeks of infection is typically called the catarrhal phase. The patient is usually most contagious during this stage of infection and signs and symptoms include nasal congestion, rhinorrhea, sneezing, and a low-grade fever. The catarrhal phase is followed by a paroxysmal phase which occurs during weeks 2-5 of infection. The paroxysmal phase is characterized by paroxysms of intense coughing lasting up to several minutes, occasionally followed by a loud inspiratory whooping sound, characteristic of this infection.
Antibiotic use can hasten the eradication of the bacteria and help prevent spread. Erythromycin is one of the preferred agents for patients aged 1 month or older.
Play Video + QuizQuestion 1 |
Mosquitoes Hint: While mosquitoes have been implemented in the spread of several infectious diseases, pertussis is not one of them. | |
Adult humans | |
Dogs and cats Hint: Contact with dogs and cats has lead to the development of upper and lower respiratory infections that are caused by Bordetella bronchiseptica, but not pertussis. | |
White-tailed deer Hint: White-tailed deer are part of the transmission cycle for Lyme disease, not pertussis. |
Question 2 |
Pertussis | |
Allergic rhinitis Hint: See A for explanation. | |
Pharyngitis Hint: See A for explanation. | |
Heart failure Hint: See A for explanation. |
Question 3 |
Macrolide prophylaxis | |
Isolation Hint: Isolation of contacts is impractical and unnecessary. | |
Observation and treatment only if symptomatic Hint: Pertussis is rarely diagnosed before the paroxysmal stage, by which time exposure of contacts to the pathogen is assured. | |
Supportive care only Hint: While supportive care is essential in those contacts with symptoms, macrolide prophylaxis is mandatory in all contacts to prevent further spread of the illness. |
Question 4 |
Azithromycin (Zithromax) | |
Ceftriaxone (Rocephin) Hint: Ceftriaxone does not eradicate Bordetella pertussis. | |
Ampicillin (Unasyn) Hint: Ampicillin may be used for macrolide-intolerant patients however it is not the drug of choice. | |
Gentamicin (Garamycin) Hint: Gentamicin does not eradicate Bordetella pertussis. |
|
List |
References: Merck Manual · UpToDate