Patient will present as → a 60-year-old female with shortness of breath of recent onset. She has a six-year history of cough and rhonchi and is on oxygen at home. Physical exam reveals a respiratory rate of 32, slightly labored breathing, and a temperature of 98.9F. Her SpO2 is 90% while receiving oxygen via nasal cannula at 2 Lpm.
Listen to her lungs (you may need to crank up the volume)
To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
One of two major presentations of chronic obstructive pulmonary disease (COPD) which includes chronic bronchitis and emphysema
- Defined by clinical features of a chronic cough that is productive of phlegm occurring on most days for 3 months of the year for two or more consecutive years without an otherwise-defined acute cause
- vs emphysema which is defined by structural changes (enlarged air spaces secondary to alveolar destruction)
- Obstruction in bronchioles due to mucus (causes air trapping, wheezing, cough, and rales) and less mobile cilia
Patients with chronic bronchitis are identified as "blue bloaters"
-
- Color indicative of hypoxia observed in the bluish tint of skin and mucous membranes
- Common in smokers (80% of COPD patients)
- The single best variable for predicting which adults will have airflow obstruction on spirometry is a history of more than 40 pack-years of smoking 95%
- Symptoms of bronchitis include coughing up mucus, wheezing, dyspnea, and chest discomfort
- Physical exam: wheezes, rales, decreased breath sounds, barrel-chested, pursed-lip breathing, productive cough, and rhonchi
Chest radiographs in chronic bronchitis demonstrate increased interstitial markings, particularly at the bases and thickening of the bronchial walls. Unlike in emphysema, diaphragms are NOT flattened
- Labs: ↑ HGB and HCT are common because of the chronic hypoxic state
- High CO2 in the blood (hypercapnia) and low O2 in the blood (hypoxemia)
- Respiratory acidosis (arterial PCO2> 45 mmHg, bicarbonate > 30 mEq/L)
- Lung biopsy (gold standard)- diagnosis is clinical but confirmed by postmortem biopsy ↑ Reid index (gland layer is > 50% of the total bronchial wall)
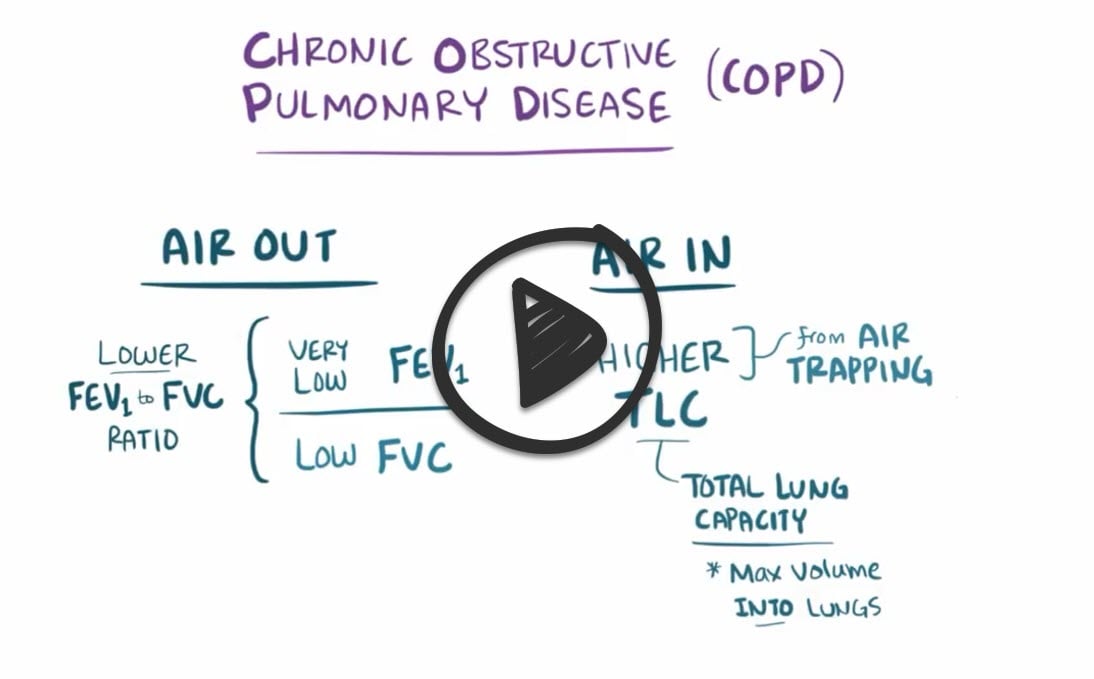
PFTs in chronic bronchitis:
FEV1/FVC ratio of < 0.7
- Airflow limitation that is irreversible or only partially reversible with a bronchodilator is the characteristic physiologic feature of COPD
- Decreased FEV1 / FVC
- Normal or decreased FVC
- Normal or increased TLC (in emphysema and asthma, specifically)
In patients with FEV1/FVC <0.70, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) system categorizes airflow limitation into stages. Determining a patient’s GOLD status requires a multidimensional assessment of a patient’s spirometry, symptom burden, and frequency of COPD exacerbations:
GOLD (spirometry)
- GOLD 1 – mild: FEV1 ≥80% predicted
- GOLD 2 – moderate: 50% ≤ FEV1 <80% predicted
- GOLD 3 – severe: 30% ≤ FEV1 <50% predicted
- GOLD 4 – very severe: FEV1 <30% predicted
Symptom burden is quantified by either the modified Medical Research Council (mMRC ) dyspnea scale (MedCalc) or COPD assessment test (CAT) score (MedCalc)
Modified Medical Research Council (mMRC) dyspnea scale
| Grade | Description of breathlessness |
| 0 | I only get breathless with strenuous exercise |
| 1 | I get short of breath when hurrying on level ground or walking up a slight hill |
| 2 | On level ground, I walk slower than people of the same age because of breathlessness, or have to stop for breath when walking at my own pace |
| 3 | I stop for breath after walking about 100 yards or after a few minutes on level ground |
| 4 | I am too breathless to leave the house or I am breathless when dressing |
GOLD status (A-D) explicitly guides therapeutic interventions
- Group A: low risk (0-1 exacerbation per year, not requiring hospitalization) and fewer symptoms (mMRC 0-1 or CAT <10)
- Group B: low risk (0-1 exacerbation per year, not requiring hospitalization) and more symptoms (mMRC ≥ 2 or CAT≥ 10)
- Group C: high risk (≥2 exacerbations per year, or one or more requiring hospitalization) and fewer symptoms (mMRC 0-1 or CAT <10)
- Group D: high risk (≥2 exacerbations per year, or one or more requiring hospitalization) and more symptoms (mMRC ≥ 2 or CAT≥ 10)
The most effective therapy for most patients with chronic bronchitis is smoking cessation
- Treatment depends on severity: a combination of short-acting (SABA) or long-acting (LABA) beta 2 agonist and short-acting (SAMA) or long-acting (LAMA) muscarinic agent (also known as an anticholinergic agent) +/- inhaled glucocorticoids
- Long-term oxygen therapy in all patients with COPD who have chronic hypoxemia defined as resting PaO2 < 55 mmHg or SaO2 < 89%
- Vaccination against both influenza and pneumococcal disease
- COPD exacerbations are managed with systemic glucocorticoids, antibiotics (tailored to the likelihood of specific pathogens), antiviral therapy when influenza is suspected
- Glucocorticoids: prednisone 40 mg per day for five days
- Antibiotics (examples):
- Azithromycin 500 mg x 3 days or Z-pack x 5 days
- Cefuroxime 500 mg BID x 10 days
- Doxycycline 100 mg BID x 10 days
Management of refractory chronic obstructive pulmonary disease
For patients with recurrent exacerbations (e.g., at least two per year or one requiring hospitalization per year) despite optimized inhaled therapies, we suggest either the phosphodiesterase-4 (PDE-4) inhibitor roflumilast or chronic azithromycin
Complications:
- The chronic hypoxic vasoconstriction from chronic bronchitis can lead to cor pulmonale (right-sided heart failure as a result of disease of the lungs or the pulmonary blood vessels)
Management of stable COPD
Initiation of therapy based on the GOLD ABCD assessment of symptoms and risk of exacerbation (source: UptoDate)
| Groups | Symptoms | Risk | Suggested treatment |
| All |
|
||
| A | Less symptomatic
Mild or infrequent symptoms (ie, breathless with strenuous exercise or when hurrying on level ground or walking up a slight hill) |
Low risk
0 or 1 exacerbations in the past year without associated hospitalization |
Short-acting bronchodilator (SABA, SAMA, or combination of SABA-SAMA), as needed. |
| B | More symptomatic
Moderate to severe symptoms (ie, the patient has to walk more slowly than others of the same age due to breathlessness, has to stop to catch breath when walking on level ground at own pace, or has more severe breathlessness) |
Low risk
0 or 1 exacerbations in the past year without associated hospitalization |
Regular treatment with a long-acting bronchodilator, either LAMA or LABA, based on patient preference. Short-acting bronchodilator (usually SABA) for symptom relief as needed. |
| C | Less symptomatic
Mild or infrequent symptoms (ie, breathless with strenuous exercise or when hurrying on level ground or walking up a slight hill) |
High risk
≥2 exacerbations per year with one or more leading to hospitalization |
Regular treatment with a LAMA; SABA available for symptom relief as needed. |
| D | More symptomatic
Moderate to severe symptoms (ie, the patient has to walk slower than others of the same age due to breathlessness, has to stop to catch breath when walking on level ground at own pace, or has more severe breathlessness) |
High risk
≥2 exacerbations per year with one or more leading to hospitalization |
Regular treatment with LAMA or, if severe breathlessness (eg, CAT >20), combination LABA plus LAMA. A combination glucocorticoid-LABA inhaler may be preferred, if features of asthma/COPD overlap. SABA available for symptom relief as needed. |
 Osmosis Osmosis |
|
 |
Chronic bronchitis a type of obstructive lung disease that is caused by chronic inflammation of the airway, which causes recurrent damage to the respiratory epithelium in the bronchi, resulting in hypertrophy of the mucus-secreting glands. This can be measured with a Reid index greater than 50%. Reid index measures the thickness of the gland divided by the total thickness of the bronchial wall. The clinical diagnostic criteria for chronic bronchitis are productive cough for greater than 3 months per year, for 2 plus years. There are two forms of COPD: chronic bronchitis and emphysema. Patients with chronic bronchitis are also referred to as blue bloaters, and patients with emphysema are referred to as pink puffers. This is because chronic bronchitis patients have early-onset hypoxemia and cyanosis (blue), but they have late-onset dyspnea. Common symptoms are signs that include wheezing and crackles and sputum production.
Play Video + QuizQuestion 1 |
Destruction of the lung parenchyma Hint: Destruction of the gas-exchanging structures in the lung is characteristic of emphysema. | |
Mucous gland enlargement and goblet cell hyperplasia | |
Smooth muscle hypertrophy in the large airways Hint: There may be smooth muscle hypertrophy in chronic bronchitis but it is not to the extent as found in asthma and is not an underlying factor in the pathology of chronic bronchitis. | |
Increased mucus adhesion secondary to reduction in the salt and water content of the mucus Hint: Abnormal absorption of sodium and a reduced rate of chloride secretion in cystic fibrosis leads to thickening of the mucus and increase in adhesion of the mucus. |
Question 2 |
1 year Hint: See C for explanation | |
3 years Hint: See C for explanation | |
5 years | |
10 years Hint: See C for explanation |
Question 3 |
Decrease the oxygen flow rate. Hint: Decreasing the oxygen flow rate would be harmful as it would decrease the amount of oxygen delivered to the patient. | |
Administer oral corticosteroids. Hint: Administration of steroids is an important treatment modality but this patient is in respiratory failure and needs more immediate therapy. | |
Intubate the patient. | |
Administer salmeterol (Serevent) Hint: Long-acting beta agonist therapy such as salmeterol is not utilized for rescue therapy. |
Question 4 |
tidal volume Hint: Tidal volume is usually unchanged, residual volume and total lung capacity are decreased with a restrictive disease pattern. This scenario presents with bronchitis which is an obstructive disease. | |
forced expiratory volume in 1 second/forced vital capacity | |
residual volume Hint: The residual volume, the volume of air left in the lungs following full expiration, is often increased in COPD, as is the total lung capacity | |
total lung capacity Hint: The residual volume, the volume of air left in the lungs following full expiration, is often increased in COPD, as is the total lung capacity |
Question 5 |
oxygen supplementation with a 100% non-rebreather mask Hint: Supplemental oxygen and positive pressure ventilation are inadequate for patients with overt respiratory failure. | |
noninvasive positive pressure ventilation (NIPPV) Hint: See A for explanation | |
endotracheal intubation and mechanical ventilation | |
emergency tracheostomy Hint: Tracheostomy is indicated for an obstructed airway. |
Question 6 |
bronchodilator therapy Hint: Bronchodilator therapy is used for symptomatic treatment in patients with COPD. | |
pulmonary rehabilitation Hint: Pulmonary rehabilitation improves quality of life, dyspnea and exercise capacity. It also has been shown to reduce the rate of hospitalization. | |
oral glucocorticosteroids Hint: Chronic use of oral glucocorticosteroids is not recommended because of an unfavorable benefit/risk ratio. | |
smoking cessation |
Question 7 |
Lung cancer Hint: While the respiratory complaints of lung cancer are associated with the location and type of primary tumor, anorexia and weight loss is seen in the majority of patients. Patients will also usually have a new cough or a change in a chronic cough and may complain of hemoptysis and nonspecific chest pain. | |
Bronchiectasis Hint: While bronchiectasis presents with a chronic cough productive of copious amounts of purulent sputum, these patients most commonly also have associated complaints of hemoptysis, weight loss and pleuritic chest pain. Examination of the lungs reveals persistent crackles at the bases. | |
Chronic bronchitis | |
Interstitial lung disease Hint: Interstitial lung disease is characterized by progressive exertional dyspnea and cough, however sputum production is minimal and the examination of the lungs reveals fine, late inspiratory crackles at the bases in the majority of patients. |
Question 8 |
sarcoidosis. Hint: Sarcoidosis, interstitial lung disease and congestive heart failure most commonly produce a restrictive pattern on spirometry with a reduction in forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) secondary to the decrease in total lung capacity (TLC), but the FEV1/FVC ratio is usually normal or increased, not decreased. | |
chronic bronchitis. | |
interstitial lung disease. Hint: See A for explanation. | |
congestive heart failure. Hint: See A for explanation. |
Question 9 |
Antibiotic | |
Inhaled corticosteroid Hint: Inhaled corticosteroids are not indicated in the management of acute exacerbations of COPD. | |
Long acting beta-agonist Hint: Long acting beta-agonists are not indicated in the management of acute exacerbations of COPD. | |
Theophylline Hint: Theophylline is rarely used in the management of COPD and has no place in the management of acute exacerbations of COPD. |
Question 10 |
Inhaled bronchodilator therapy Hint: Inhaled bronchodilators afford symptomatic relief for some patients with COPD but do not alter the disease course. | |
Inhaled steroid therapy Hint: Inhaled steroid therapy may reduce the number and severity of COPD exacerbations but has not been shown to alter the disease course. | |
Home oxygen | |
Theophylline Hint: Theophylline is a third-line agent for treating COPD and will not alter the natural history of the disease |
Question 11 |
Centriacinar emphysema | |
Panacinar emphysema | |
Distal acinar emphysema | |
Paraseptal emphysema |
Question 12 |
Asthma | |
Bronchiectasis | |
Underweight status | |
Depression |
Question 13 |
Productive cough | |
Pulmonary hypertension | |
Cor pulmonale | |
Breathlessness |
Question 14 |
Serum chemistry evaluation | |
Alpha1-antitrypsin measurement | |
Arterial blood gas (ABG) analysis | |
Sputum evaluation |
Question 15 |
Pneumococcal vaccines are contraindicated in patients with COPD | |
Intravenous alpha1-antitrypsin levels should be kept at 8-10 mmol/L | |
Long-term oxygen therapy is recommended for patients with a partial pressure of oxygen in arterial blood <55 mm Hg or oxygen saturation <90% | |
Because cardiovascular disease is common in patients with COPD, beta-blockers are indicated in all patients |
Question 16 |
No demonstrable abnormality Hint: Spirometry findings in obstructive lung disease typically show normal or increased total lung capacity, decreased vital capacity, prolonged FEV1, and increased residual volume. | |
Restrictive lung disease Hint: Restrictive lung disease would show decreased total lung capacity, vital capacity, and normal to increased FEV1. | |
Obstructive lung disease | |
A ventilation/perfusion mismatch Hint: A ventilation/perfusion scan would be abnormal with a pulmonary embolism. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture




