68 y/o female with 6 months of bilateral chest pain and difficulty breathing
Patient presents as → a 58-year-old female who returns to the hospital with chest pain and difficulty breathing several weeks after being discharged following a myocardial infarction requiring immediate cardiac catheterization. She has been coughing up frothy sputum for the past three days. The patient complains of a sharp pain that worsens during inspiration. Physical exam reveals decreased tactile fremitus, dullness to percussion, and diminished breath sounds on the left side. Chest X-ray demonstrates blunting of the left costophrenic angle, meniscus sign, obliteration of the left hemidiaphragm, and mediastinal shift.
To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
A pleural effusion is a pathologic accumulation of fluid in the pleural space (often associated with pneumonia)
- Presents with decreased breath sounds + decreased tactile fremitus
Tactile fremitus refers to the palpable vibration of the chest wall that results from the transmission of sound vibrations through the lung tissue to the chest wall
| Decreased tactile fremitus | Increased tactile fremitus |
Decreased intensity of tactile fremitus may occur as a result of the following:
|
Increased intensity of tactile fremitus generally occurs as a result of increased density within the lung tissue
|
- Transudate = think “transient” fluid due to hydrostatic pressure (cirrhosis, CHF, nephrotic syndrome)
- The most common causes of transudative effusions are heart failure, cirrhosis with ascites, and hypoalbuminemia (usually due to nephrotic syndrome)
- Exudative = fluid due to infection (pneumonia), malignancy, immune
- The most common causes of exudative effusions are pneumonia, cancer, pulmonary embolism, and tuberculosis
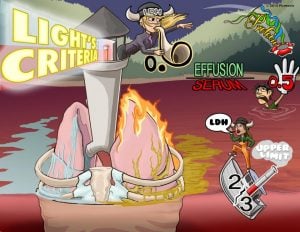
Light's criteria: If at least one of the following three criteria is present, the fluid is defined as an exudate
Basically, ↑ Protein and ↑ LDH = Exudative
- Pleural fluid protein/serum protein ratio > 0.5
- Pleural fluid LDH/serum LDH ratio greater than 0.6
- The pleural fluid LDH is greater than two-thirds the upper limit of normal for serum LDH
“It's all about that LDH"
Evaluation requires imaging (usually chest x-ray) to confirm the presence of fluid and pleural fluid analysis to help determine the cause
- Lateral decubitus chest x-ray, chest CT, or ultrasonography should be done if it is unclear whether an x-ray density represents fluid or parenchymal infiltrates or whether the suspected fluid is loculated or free-flowing
- A large free pleural effusion appears as a dependent opacity with lateral upward sloping of a meniscus-shaped contour at the junction of the lung and the diaphragm (meniscus sign). The diaphragmatic contour is partially or completely obliterated, depending on the amount of the fluid (silhouette sign)
Physical exam: decreased tactile fremitus and dullness to percussion would be found in a pleural effusion
- In pleural effusions, vocal fremitus is decreased
- In pleural effusions, breath sounds are decreased
- Isolated left-sided pleural effusion is likely exudative
- Right-sided think transudative
Treatment is with thoracocentesis
- Small transudative pleural effusions resulting from heart failure may be treated with diuretics and sodium restriction
- Effusions that are chronic or recurrent and causing symptoms can be treated with pleurodesis (pleural space is artificially obliterated) or by intermittent drainage with an indwelling catheter
 Osmosis Osmosis |
|
 |
Light’s Criteria is a diagnostic tool used to determine if the cause of a pulmonary effusion; transudate versus exudate. This relies on a comparison of the chemistries in the pleural fluid to those in the blood. According to Light’s criteria, a pleural effusion is likely exudative if at least one of the following exists: The ratio of pleural fluid protein to serum protein is greater than 0.5, the ratio of pleural fluid LDH and serum LDH is greater than 0.6, or the pleural fluid LDH is greater than 0.6 or 2⁄3 times the normal upper limit for serum.
Play Video + QuizQuestion 1 |
asthma Hint: Asthma is characterized by decreased tactile fremitus, but would have resonant to hyperresonant percussion, not dullness. | |
consolidation Hint: Consolidation from pneumonia is characterized by dullness to percussion, but would have an increased, not decreased, tactile fremitus. | |
pneumothorax Hint: A pneumothorax is characterized by decreased to absent tactile fremitus, but would have a hyperresonant percussion note, not dullness. | |
pleural effusion |
Question 2 |
Kaposi's sarcoma Hint: Kaposi's sarcoma, pneumonia, or mesothelioma will produce a transudative pleural effusion. | |
Pneumonia Hint: See A for explanation. | |
Cirrhosis | |
Mesothelioma Hint: See A for explanation. |
Question 3 |
Thoracotomy Hint: A thoracotomy is indicated in a small percentage of patients that do not respond to IV administration of fluids and evacuation of the hemothorax via tube thoracostomy.
(u) B. Needle aspiration as treatment for a hemothorax is not recommended as it fails to adequately drain the bloody fluid. | |
Needle aspiration Hint: Needle aspiration as treatment for a hemothorax is not recommended as it fails to adequately drain the bloody fluid. | |
Close observation Hint: Close observation is only indicated for small effusions in a patient that remains hemodynamically stable. | |
Tube thoracostomy |
Question 4 |
Repeat chest x-ray in two months Hint: See B for explanation. | |
Perform diagnostic thoracentesis | |
Order MRI of the chest Hint: See B for explanation. | |
Treat with antibiotic Hint: See B for explanation. |
Question 5 |
Hyperresonance to percussion Hint: Hyperresonance to percussion would be suggestive of emphysema or pneumothorax | |
Increased tactile fremitus Hint: Increased tactile fremitus would be consistent with a consolidation. | |
Unilateral lag on chest expansion | |
Egophony Hint: Though egophony may be present with pleural effusion it is only heard above the level of the effusion in an upright patient. The presence of egophony would be most consistent with consolidation. |
Question 6 |
Pleural fluid protein/serum protein ratio < 0.5 Hint: A pleural fluid protein/serum protein ratio less than 0.5 would be consistent with a transudative effusion. | |
Pleural fluid LDH/serum LDH ratio < 0.6 Hint: A pleural fluid LDH/serum LDH ratio less than 0.6 would be consistent with a transudative effusion. | |
Pleural fluid cholesterol < 45 mg/dL Hint: Pleural fluid cholesterol is not one of Light’s criteria for differentiating between exudative and transudative effusions. | |
Pleural fluid protein/serum protein ratio > 0.5 | |
Pleural fluid LDH < two-thirds the upper limit of normal for serum LDH Hint: A pleural fluid LDH less than two-thirds the upper limit of normal for serum LDH would be consistent with a transudative effusion. |
- The pleural fluid protein/serum protein ratio is greater than 0.5
- The pleural fluid LDH/serum LDH ratio is greater than 0.6
- The pleural fluid LDH is greater than two-thirds the upper limit of normal for serum LDH
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture