Patient will present as → a 43-year-old woman with a history of COPD presents to your office with worsening dyspnea, especially at rest. She also complains of dull, retrosternal chest pain. On examination, she has persistent widened splitting of S2. Radiographic findings demonstrate peripheral “pruning” of the large pulmonary arteries.
**Peripheral “pruning” of the large pulmonary arteries is characteristic of pulmonary hypertension in severe emphysema
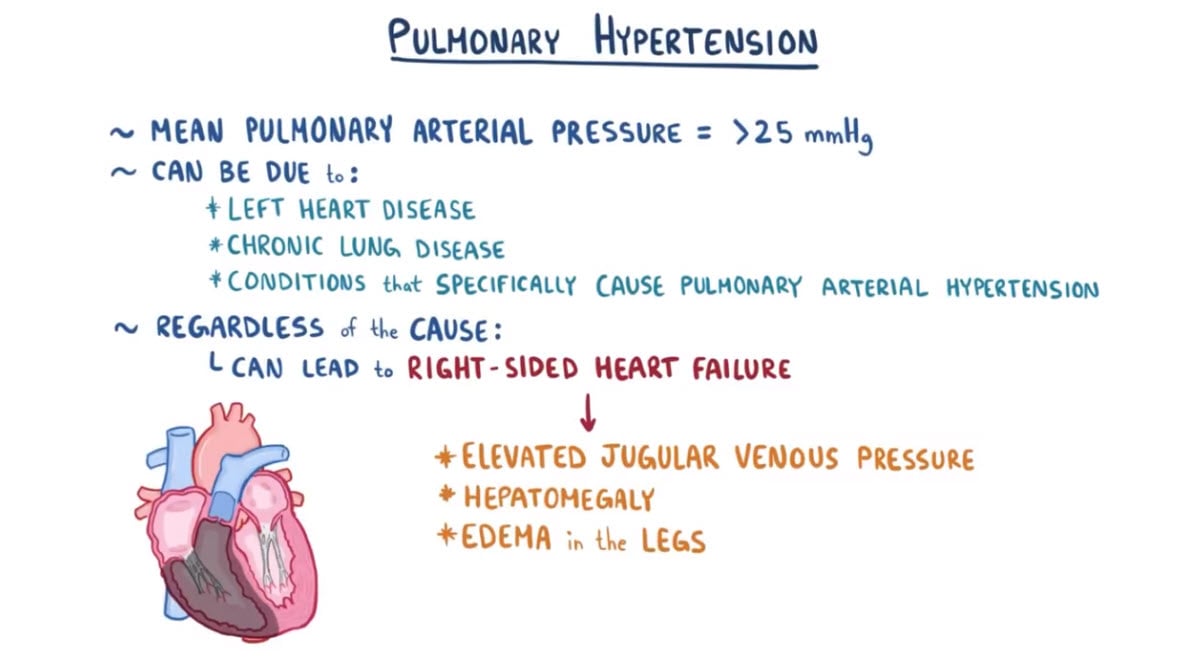
Blood pressure in the lungs is usually very low 15/5. In pulmonary hypertension, the pressure increases > 20 mmHg at rest
- It can be due to left heart disease, chronic lung disease, or conditions that specifically cause pulmonary arterial hypertension.
- Mitral stenosis is the most common cause of pulmonary HTN due to a cardiac problem. The mitral valve is so tight blood can't pass into the left ventral, which backs pressure up into the lungs.
- The pressure can become so great that the right heart can no longer pump against the vascular resistance, which leads to right heart failure and Cor Pulmonale
- Pulmonary Arterial Hypertension
- Pulmonary Hypertension due to left heart disease
- Pulmonary Hypertension due to lung disease
- Pulmonary Hypertension due to blood clots in the lungs
- Blood and other rare disorders that lead to Pulmonary Hypertension
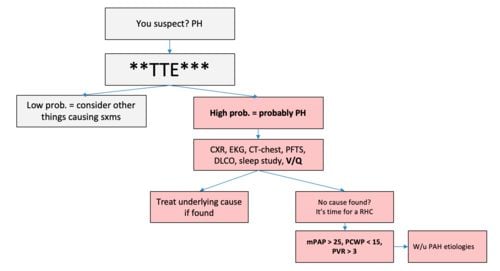
Pulmonary hypertension is difficult to diagnose early on as signs and symptoms are often related to the underlying cause
- Transthoracic echocardiogram (first diagnostic test for pulmonary HTN)
- Increased pressure in pulmonary arteries, right ventricles → dilated pulmonary artery
- Dilatation/hypertrophy of right atrium, right ventricle
- Large right ventricle → bulging septum
- Right heart catheterization is the GOLD STANDARD for diagnosis of pulmonary HTN → most accurate measure of pressures
- Chest X-Ray - The classic findings on chest radiography in a patient with pulmonary arterial hypertension include enlarged central pulmonary arteries that taper distally (peripheral pruning), attenuated peripheral vessels, and oligemic lung fields.
- ECG → Right heart strain pattern: T wave inversion in right precordial (V1–V4), and inferior leads (II, III, aVF)
Diagnostic algorithm for pulmonary hypertension
Identify and treat the underlying cause
- Pulmonary hypertension secondary to left ventricular failure → optimize left ventricular function
- Diuretics (cautiously—individuals may be preload dependent)
- Digoxin
- Anticoagulants
- Cardiogenic pulmonary arterial hypertension
- Relax smooth muscle (promote vasodilation), reduce vascular remodeling, improve exercise capacity with prostanoids, phosphodiesterase inhibitors, endothelin antagonists
- Pulmonary arterial hypertension
- Endothelin receptor antagonists
- Prostanoids
Question 1 |
right heart catheterization | |
spirometry Hint: Patients initially undergo chest x-ray, spirometry, and ECG to identify more common causes of dyspnea, | |
chest X-ray Hint: Patients initially undergo chest x-ray, spirometry, and ECG to identify more common causes of dyspnea, | |
echocardiography Hint: pulmonary artery pressure is estimated by echocardiography |
Question 2 |
90 mmHg Hint: See D for explanation. | |
80 mmHg Hint: See D for explanation. | |
70 mmHg Hint: See D for explanation. | |
60 mmHg |
Question 3 |
≥ 5 mm Hg Hint: See D for explanation | |
≥ 10 mm Hg Hint: See D for explanation | |
≥ 15 mm Hg Hint: See D for explanation | |
≥ 25 mm Hg |
|
List |
References: Merck Manual · UpToDate


 Osmosis
Osmosis