The NCCPA™ PANCE Pulmonary Content Blueprint other pulmonary diseases
| Acute respiratory distress syndrome (ARDS) | Patient will present as → a patient brought to the emergency room with acute onset of dyspnea and tachypnea. He has a long history of alcoholism and was involved in a motor vehicle accident two days ago. He is hypoxic with crackles auscultated bilaterally and frothy pink sputum. Chest radiography reveals diffuse bilateral infiltrates, which spare the costophrenic angle and air bronchograms. There is no cardiomegaly or pleural effusion noted. Oxygen saturation is 70%. Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by fluid collecting in the lungs, depriving organs of oxygen
People with ARDS have severe shortness of breath and often are unable to breathe on their own without support from a ventilator
Chest radiograph shows air bronchograms and bilaterally fluffy infiltrate
Treatment involves identifying and managing underlying conditions
|
| Asthma (ReelDx) | Patient will present as → a 5-year-old boy who is brought to the emergency department by his parents for a cough and shortness of breath. He has a past medical history of eczema and seasonal rhinitis. On physical exam, you note a young boy in respiratory distress taking deep, slow breaths to try and catch his breath. He has diminished breath sounds in all lung fields with prolonged expiratory wheezes. ReelDx Virtual Rounds (asthma)Presentation: Most often, young patients present with wheezing and dyspnea often associated with illness, exercise, and allergic triggers Diagnosis and monitor with peak flow. PFTs: Greater than 12% increase in FEV1 after bronchodilator therapy
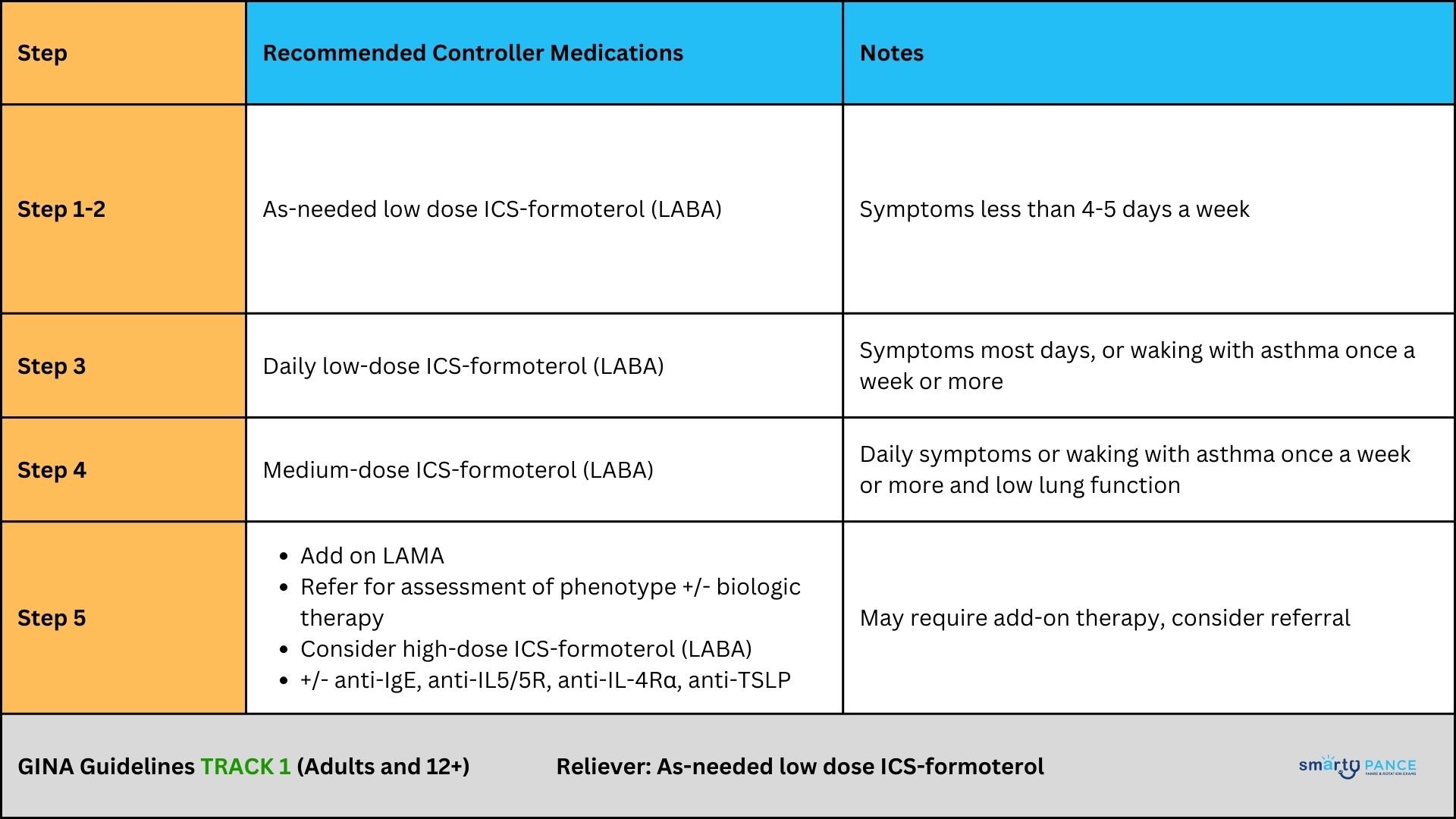
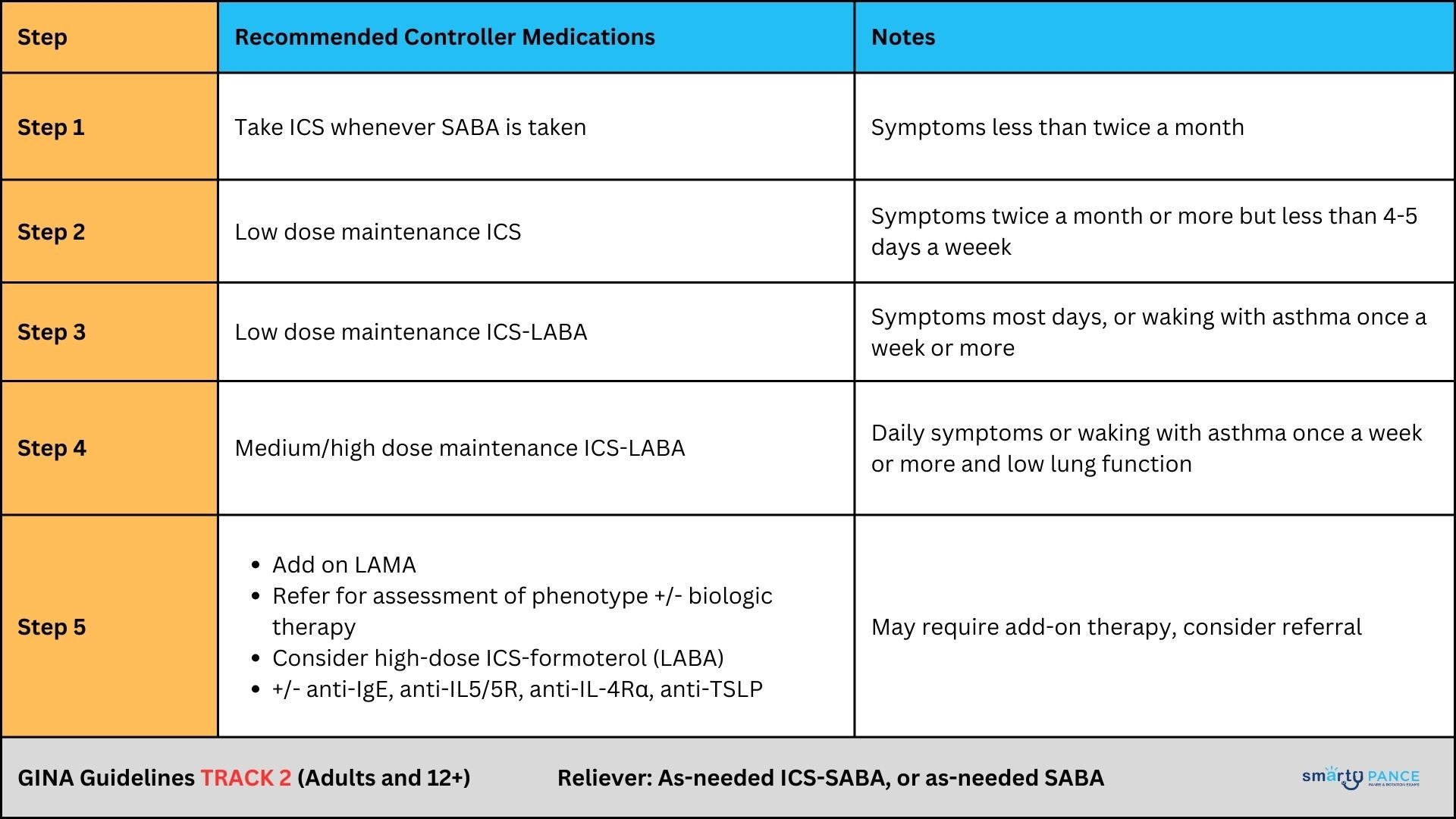
Treatment guidelines: The 2023 GINA strategy divides asthma treatment into two tracks for adults and adolescents:
Table 1: GINA Track 1
Table 2: GINA 2023 Track 2
Acute treatment: Oxygen, nebulized SABA, ipratropium bromide, and oral corticosteroids Making Sense of Forced Vital Capacity
|
| Cystic fibrosis | Patient will present as → a 7-year-old boy brought by his parents due to a persistent cough, wheezing, and recurrent lung infections since infancy. The parents also report the child having bulky, foul-smelling stools and difficulty gaining weight despite a good appetite. On examination, he appears underweight, with digital clubbing and crackles heard on lung auscultation. His growth chart shows him below the 3rd percentile for his age. A sweat chloride test shows a chloride level of 88 mmol/L (normal <40 mmol/L). His stool elastase test is low, indicating pancreatic insufficiency. Genetic testing confirms the diagnosis of cystic fibrosis with the identification of mutations in the CFTR gene. Cystic fibrosis affects the cells that produce mucus, sweat, and digestive juices. It causes these fluids to become thick and sticky. They then plug up tubes, ducts, and passageways. Etiology: Autosomal recessive mutation in the CFTR gene
Presentation: Recurrent respiratory infections (especially Pseudomonas), steatorrhea Diagnosis: Quantitative sweat chloride test CXR may reveal hyperinflation, mucus plugging, and focal atelectasis Treatment:
A 12-year-old girl with cystic fibrosis. a The AP radiograph shows mild to moderate general changes of cystic fibrosis, with increased linear markings and discrete nodular opacities (arrowheads) in the periphery of both lungs. Bronchiectases are suspected in the upper parts of both hilar regions (white arrows). b A tomosynthesis section |
| Foreign body aspiration | ReelDx Virtual Rounds (Foreign body aspiration)Patient will present as → a 2-year-old male child who is brought to the emergency department by his mother with a sudden onset of choking, gagging, coughing, and wheezing. Vital signs are temperature 37 ° C, pulse 120/min, and respirations 28/min. The physical examination reveals decreased breath sounds over the right lower lobe with inspiratory rhonchi and localized expiratory wheezing. The chest X-ray reveals normal inspiratory views, but expiratory views show localized hyperinflation with a mediastinal shift to the left. Foreign body aspiration occurs when a foreign body enters the airways and causes choking. Objects can enter the esophagus through the mouth or enter the trachea through the mouth or nose
Presentation (depends on the location of obstruction)
CXR (expiratory radiograph) may reveal regional hyperinflation of the affected side
Treatment: Remove foreign body with a bronchoscope
|
| Hyaline membrane disease | Patient will present as → a premature infant who is born at 32 weeks and, after several hours, develops rapid shallow respirations at 60/ min, grunting retractions, and duskiness of the skin. The chest X-ray reveals diffuse bilateral atelectasis, ground glass appearance, and air bronchograms. Hyaline membrane disease (HMD), also called neonatal respiratory distress syndrome (RDS), is a condition in newborn babies in which the lungs are deficient in surfactant, preventing their proper expansion and causing the formation of hyaline material in the lung spaces Etiology: Insufficient surfactant
Treatment: Ventilation and steroids Acute respiratory distress syndrome (ARDS) vs. Hyaline membrane disease/newborn respiratory distress syndrome (RDS)
|
| Bronchiectasis | Patient will present as → a 25-year-old cystic fibrosis patient complaining of chronic, frequent coughing productive of yellow and green sputum. She recently recovered from a Pseudomonas spp. Pneumonia requiring hospitalization. On physical examination, you notice foul breath, purulent sputum, and hemoptysis, along with a CXR demonstrating dilated and thickened airways with “plate-like” atelectasis (scarring). A condition in which the lungs' airways become dilated and damaged, leading to inadequate clearance of mucus in airways
DX: CXR = linear “tram track” lung markings, dilated and thickened airways – “plate-like” atelectasis
TX: ambulatory oxygen, aggressive antibiotics for acute exacerbations, CPT (chest physiotherapy = bang on the back); eventual lung transplant |