Intermittent obstruction of the airflow (typically at the level of the oropharynx) produces periods of apnea during sleep
- Each apneic period is usually 20 to 30 seconds long (but may be longer) and results in hypoxia, which arouses the patient from sleep. This occurs multiple (sometimes hundreds of) times overnight.
Risk factors
- Obesity (especially around the neck): nonobese patients can also have OSA
- Structural abnormalities: enlarged tonsils, uvula, soft palate; nasal polyps; hypertrophy of muscles in the pharynx; deviated septum; deep overbite with a small chin
- Family history
- Alcohol and sedatives worsen the condition
- Hypothyroidism (multifactorial)
Presents as:
- Snoring and daytime sleepiness due to disrupted nocturnal sleep
- Personality changes, decreased intellectual function, decreased libido, morning headaches, polycythemia
- Repeated oxygen desaturation and hypoxemia can lead to systemic and pulmonary HTN as well as cardiac arrhythmias
Obesity-hypoventilation syndrome (OHS) (historically described as the Pickwickian syndrome)
- Consists of the triad of obesity (BMI > 30), sleep-disordered breathing, and chronic hypercapnia (PCO2 > 45 mmHG) during wakefulness in the absence of other known causes of hypercapnia
- Signs and symptoms of obesity hypoventilation syndrome (OHS) are essentially the same as OSA. These two diseases are often concurrent.
Polysomnography (overnight sleep study in a sleep laboratory) confirms the diagnosis of obstructive sleep apnea and can distinguish OSA from CSA
- Home sleep apnea testing (HSAT) may be an acceptable alternative for patients who are strongly suspected of having OSA and who do not have medical comorbidities (eg, heart failure or lung disease)
In adults, a diagnosis of OSA is defined by either of the following:
Five or more predominantly obstructive respiratory events per hour of sleep (for polysomnography) or recording time (for HSAT) in a patient with one or more of the following:
- Sleepiness, nonrestorative sleep, fatigue, or insomnia symptoms
- Waking up with breath-holding, gasping, or choking
- Habitual snoring, breathing interruptions, or both noted by a bed partner or other observer
- Hypertension, mood disorder, cognitive dysfunction, coronary artery disease, stroke, congestive heart failure, atrial fibrillation, or type 2 diabetes mellitus
Fifteen or more predominantly obstructive respiratory events per hour of sleep (for polysomnography) or recording time (for OCST), regardless of the presence of associated symptoms or comorbidities
Obesity-hypoventilation syndrome (OHS) is a diagnosis of exclusion that can be made when the following criteria are met:
- Obesity (body mass index [BMI] >30 kg/m2)
- Awake alveolar hypoventilation as indicated by a partial arterial pressure of carbon dioxide >45 mmHg
- Alternative causes hypercapnia and hypoventilation have been excluded
Management of obstructive sleep apnea
Behavior/lifestyle modification for ALL patients who have OSA and a modifiable risk factor
- This includes weight loss and exercise, avoiding alcohol and sedatives, smoking cessation, and sleeping in a non-supine position
Mild to moderate OSA:
- Positive airway pressure therapy
- If the patient refuses or there are issues with compliance, an oral appliance can be offered
Severe OSA:
- Continuous positive airway pressure (CPAP) provides positive pressure, thus preventing occlusion of the upper pharynx. This is the preferred therapy for the majority of patients because it is noninvasive and has proven efficacy. It is poorly tolerated by some due to noise and discomfort
- Uvulopalatopharyngoplasty—removal of redundant tissue in the oropharynx to allow more airflow
- Tracheostomy is a last resort for those in whom all other therapies have failed or who have life-threatening OSA (severe hypoxemia or arrhythmias)
Management of obesity hypoventilation syndrome
- Weight loss +/- CPAP at night
- For patients with OHS who fail or do not tolerate first-line therapies in whom aggressive attempts have been made to optimize PAP therapy, options include tracheostomy for the treatment of sleep-disordered breathing and bariatric surgery or rarely medication for weight loss
 Osmosis Osmosis |
|
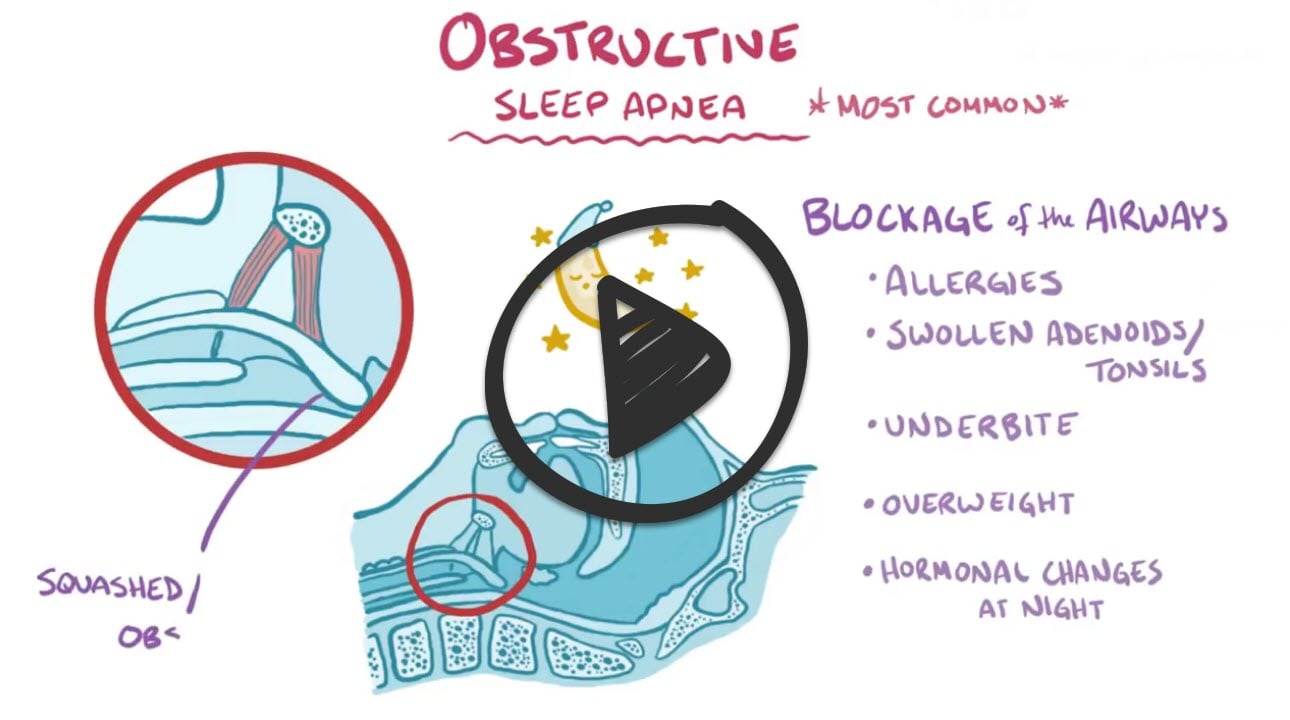 |
Obstructive sleep apnea (OSA) is caused by narrowing or obstruction of the airway during sleep. A patient diagnosed with this disorder will experience five or more episodes of apnea per hour. When a patient becomes hypercapnic due to periods of apnea, they will experience a startle response, in the form of a snort or a gasp, which allows the tongue and soft palate to fall forward, thereby reopening the patient’s airway. Loud, frequent snoring, daytime sleepiness, and headaches are also common clinical manifestations in those with OSA. Complications of untreated sleep apnea include hypertension, right-sided heart failure from pulmonary hypertension, and cardiac dysrhythmias. Interventions to treat obstructive sleep apnea include changing the patient’s sleeping position, use of an oral appliance such as a mouth guard, CPAP, BiPAP, or surgical interventions. Patients with OSA should be encouraged to lose weight, as being overweight or obese worsens sleep apnea.
Play Video + QuizQuestion 1 |
narcolepsy | |
obstructive sleep apnea (OSA) syndrome | |
generalized poor physical condition | |
central sleep apnea syndrome | |
adult-onset adenoid hypertrophy |
Question 2 |
collapse of the pharyngeal walls repetitively during sleep | |
failure of upper airway dilator muscle activity | |
sleep-related upper airway obstruction and cessation in ventilation (apneas) | |
a, b, and c |
Question 3 |
hypoxemia | |
hypercarbia | |
metabolic acidosis | |
respiratory acidosis | |
a, b, and d |
Question 4 |
systemic hypertension | |
inhibited sexual desire | |
depression | |
all of the above |
Question 5 |
alcohol intake | |
benzodiazepines | |
hyperthyroidism | |
a and b | |
all of the above |
Question 6 |
uvulopalatopharyngoplasty surgery (UPP) | |
tracheostomy | |
continuous positive airway pressure (CPAP) | |
nortriptyline | |
alprazolam |
|
List |
References: Merck Manual · UpToDate



