The NCCPA™ PANCE Pulmonary Content Blueprint covers two obstructive pulmonary diseases
You must be able to quickly differentiate between chronic bronchitis vs. emphysema
- Chronic bronchitis is defined by clinical features (chronic cough) vs. emphysema, which is defined by structural changes (enlarged air spaces secondary to alveolar destruction)
| Condition | Summary | Key Differentiators |
|---|---|---|
| Chronic Bronchitis | A form of COPD defined as a chronic, productive cough that occurs most days for three months of the year for two or more consecutive years without an otherwise-defined acute cause. | Chronic cough, sputum production, smokers, "Blue Bloaters," stocky and overweight, barrel chest, pneumonia, ↓ FEV1/FVC ratio (<0.7), peribronchial and perivascular markings, hemoglobin and hematocrit, crackles and wheezes. |
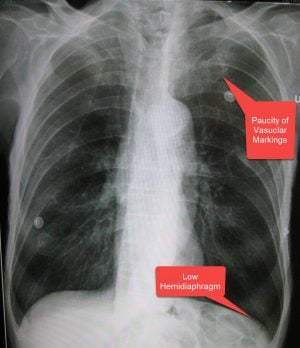
| Emphysema | A form of COPD characterized by enlargement of air spaces and destruction of alveolar septae, often resulting in a barrel-chested appearance. | Minimal cough and sputum production but more shortness of breath, "Pink Puffers," thin and underweight, loss of lung markings, hyperinflation, flattened diaphragm, small, thin-appearing heart, ↓ FEV1/FVC ratio (<0.7), parenchymal bullae, diminished breath sounds, prolonged expirations, diminished heart sounds, chronic hyperventilation, retention of CO2. |
| Chronic bronchitis | Patient will present as → a 56-year-old female with shortness of breath, as well as a productive cough that has occurred over the past two years for at least three months each year. She is a heavy smoker. Physical exam reveals a respiratory rate of 32, slightly labored breathing, and a temperature of 98.9F. Her SpO2 is 90% while receiving oxygen via nasal cannula at 2 Lpm. It is defined as a chronic cough that is productive of phlegm occurring on most days for 3 months of the year for 2 or more consecutive years without an otherwise defined acute cause
"The common organisms causing pneumonia in patients with COPD are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Patients who smoke are often colonized with Haemophilus influenza." DX:
Treatment:
|
| Emphysema | Patient with emphysema will present as → a 65-year-old male complaining of fatigue and shortness of breath with exertion. The patient reports minimal cough. On physical exam, you note a thin, barrel-chested man with decreased heart and breath sounds, pursed-lip breathing, end-expiratory wheezing, and scattered rhonchi. Chest X-ray reveals a flattened diaphragm, hyperinflation, and a small, thin-appearing heart. PFTs show a decreased FEV1/FVC ratio. Emphysema is a condition in which air spaces are enlarged as a consequence of the destruction of alveolar septae
DX:
Management is the same as Chronic Bronchitis
|
Obstructive lung disease is characterized by airway obstruction and associated with inflammation of the airways. Air trapping as a result of airway obstruction causes an increase in the residual volume of the lungs, which means the volume of air left in the lungs after fully exhaling is increased. Forced vital capacity, the volume of air that can be forcibly blown out after one full inspiration, is decreased. FEV1, the forced expiratory volume in 1 second or the volume of air that can be forcibly blown out in 1 second, is also decreased. More importantly, the ratio of FEV1/FVC is decreased because even though FVC is decreased, the FEV1 decreases even greater resulting in an overall decrease in the FEV1/FVC ratio. This can be clearly distinguished from restrictive lung disease which has a ratio greater than 80%. Common obstructive lung diseases include chronic bronchitis, emphysema, asthma, and bronchiectasis.
Play Video + QuizReferences: Merck Manual · UpToDate