90 y/o with cough and fever
Patient will present as → a 71-year-old male who was admitted to the acute care hospital two days following a massive CVA with a possible brainstem infarct. Because he was also experiencing secondary respiratory failure, he was intubated and placed on mechanical ventilation. He was subsequently transferred to the neurointensive care unit, where he was stabilized. His present vital signs are respiratory rate 14 (ventilator rate), temperature 100.4 F. His SpO2 is 95%. His rating on the Glasgow Coma Scale is 5.
To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Patients will present with fever, dyspnea, tachycardia, tachypnea, cough +/- sputum
Presentation and risk factors depend on the etiology
- S. Pneumoniae: Rust-colored sputum, common in patients with splenectomy
- S. Aureus: Salmon-colored sputum, lobar, after influenza, MRSA treat with vancomycin
- Pseudomonas: Ventilators, Cystic fibrosis, patients become sick fast - treat with 2 antibiotics
- Legionella: Air conditioning, aerosolized water, low NA+ (hyponatremia), GI symptoms (diarrhea), and high fever
- Mycoplasma: Young people living in dorms, (+) cold agglutinins, bullous myringitis, walking pneumonia, low temp
- Klebsiella: Alcohol abuse, currant jelly sputum, aspiration
- Pneumocystis jiroveci HIV CD4 <200, immunosuppressed
- Haemophilus influenzae: COPD, smokers, postsplenectomy
- Histoplasma capsulatum caused by bat droppings -looks like sarcoidosis on CXR
- Coccidioides (valley fever) in dry states
- Chlamydia pneumoniae: College kids, sore throat, long prodrome
- Poor dental hygiene is associated with pneumonia caused by anaerobes
- Influenza pneumonia is characterized by a more precipitous onset and fulminant course
- An indolent course suggests atypical pneumonia - Mycoplasma is the most common atypical agent
- Lobar consolidation is seen in community-acquired pneumonia
- Apical infiltration is seen in tuberculosis
Patients with pneumonia will have physical exam finding of
- (+) egophony - Transmission of vocal sounds through consolidation leads to the changes heard with egophony.
- (+) tactile fremitus - Consolidation would increase the transmission of vocal vibrations and manifest as increased tactile fremitus.
- (+) dullness to percussion
Empyema is the accumulation of pus in the pleural space - It is a known complication of pneumonia. The risk of this complication increases in patients with COPD, diabetes, GERD, and pleural effusions.
Outpatient therapy (antibiotics)
- Low risk or no comorbidities and low risk for P. Aerugino aeruginosa or MRSA
- Amoxicillin 1 g PO TID x 5 days
- Doxycycline 100 mg P BID x 5 days
- Azithromycin 500 PO once, then 250 mg PO daily x 4 days (if local pneumococcal resistance is < 25%)
- Significant comorbidities (chronic heart, lung, liver, or renal disease, diabetes, EtOH, active cancer, immunosuppression, asplenia)
- Amoxicillin/clavulanate (Augmentin) 875 BID or Cefuroxime 500 mg PO BID PLUS Azithromycin 500 PO once, then 250 mg PO daily x 4 days or Doxycycline 100 mg BID x 5 days
- Levofloxacin 750 mg PO daily x 5 days
- Moxifloxacin 400 mg PO daily x 5 days
Inpatient (hospitalize if > 50 with comorbidities, altered mental status, poor fluid status)
- Treatment regimens depend on various factors, which include severity, prior hospitalization, and prior abx use. Common options include:
- Ceftriaxone + Doxycycline or Azithromycin
- Levofloxacin, Moxifloxacin, Cefepime, Piperacillin/Tazobactam, Vancomycin, and Meropenem (alone and in various combinations)
 Osmosis Osmosis |
|
 |
| Picmonic | |
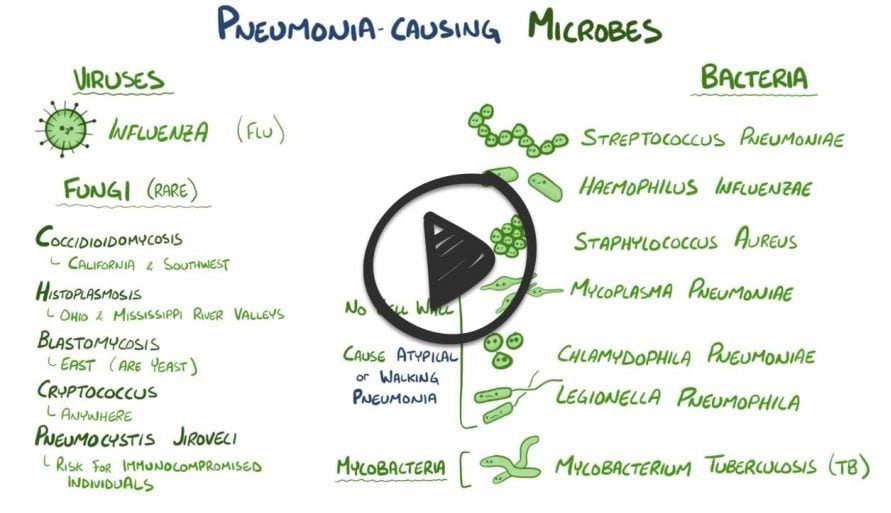
| Pneumonia is an acute or chronic lung condition defined as inflammation of the alveoli or filling of the alveoli with fluid. It is usually caused by bacteria, fungi, viruses and sometimes by physical and chemical irritants. It typically presents with fever, chest congestion, difficulty breathing, cough, and sputum. | |
 |
Rhonchi develops due to airway obstruction, increased secretions, and bronchospasms. Rhonchi can be auscultated near the trachea and bronchi and sound like a low pitched rumbling and gurgling sound. Play Video + Quiz |
 |
Crackles are caused by sudden reinflation of groups of alveoli or disruptive passage of air through small airways. Fine crackles are high-pitched and heard during the end of inspiration. Coarse crackles are loud, bubbly sounds heard during inspiration. Play Video + Quiz |
 |
Common Causes of Pneumonia: Neonates (less than 4 Weeks Old) - In neonates, common causes of pneumonia include Group B Streptococci and E. coli Play Video + Quiz |
 |
Common Causes of Pneumonia: Children (4 Weeks - 18 Years) - In middle-aged adults, common causes include Streptococcus pneumoniae, Haemophilus influenzae, anaerobes, viruses, and Mycoplasma Play Video + Quiz |
 |
Common Causes of Pneumonia: Adults (18 - 40 Years Old) - In adults ages 18-40 years, common causes of pneumonia include Mycoplasma, Chlamydia pneumoniae and Streptococcus pneumoniae. Play Video + Quiz |
 |
Common Causes of Pneumonia: Middle-Aged Adults (40 - 65 Years Old) - In middle-aged adults, common causes include Streptococcus pneumoniae, Haemophilus influenzae, anaerobes, viruses, and Mycoplasma Play Video + Quiz |
 |
Common Causes of Pneumonia: Elderly (65+ Years Old) - In older adults common causes are Streptococcus pneumoniae, influenza virus, anaerobes, H. influenzae, and gram-negative rods. Play Video + Quiz |
 |
Streptococcus pneumoniae is a gram-positive, lancet-shaped diplococci that is a major cause of pneumonia, meningitis, and otitis media in individuals. Pneumonia caused by this bacterial pathogen causes a rusty sputum, which can help with clinical diagnosis. The bacteria can also cause acute bacterial sinusitis, and can cause sepsis in patients with splenectomies Play Video + Quiz |
 |
Legionella is a gram-negative bacilli named after an outbreak among people attending a convention of the American Legion. Although the bacteria is characterized as a gram-negative bacteria, is often difficult to visualize due to poor gram staining. It requires special medium for growth called charcoal yeast extract. Legionella requires special medium because it requires the presence of iron and cysteine to grow, which is not in common blood agar media and can be readily visualized with silver stain. Legionella is known to be water loving and transmitted via inhalation of mist droplets containing bacteria. Common sources include cooling towers, hot water systems, and fountains. Individuals that are smokers, over 65 years of age, and heavy drinkers are at moderately increased risk of disease. In patients, the organism is commonly detected in the urine using the Legionella Urinary Antigen. Play Video + Quiz |
 |
Mycoplasma pneumoniae is a small bacterium with a unique cell structure that causes mycoplasma pneumonia. This species lacks a peptidoglycan cell wall, and instead has a cell membrane with sterol compounds that it obtains from the host serum. Because it requires sterols for replication, it requires special growing medium called Eaton's agar, and also has a distinctive growth pattern, forming characteristic mulberry colonies. This organism causes mycoplasma pneumonia, also known as walking pneumonia, which is an atypical pneumonia spread through respiratory droplet transmission. It is called an atypical pneumonia because there is a protracted course, lack of sputum production, and extra-pulmonary symptoms as compared to typical pneumonia. This form of pneumonia is more common in adolescents and people in close quarters like military recruits. Mycoplasma pneumonia is also characterized by the presence of IgM antibodies directed against red blood cells, leading to a cold autoimmune hemolytic anemia in some patients. Complications of this disease also include erythema multiforme, which can progress to Stevens-Johnson syndrome. Because the causative organism lacks a cell wall, it does not gram stain and is also resistant to the effects of penicillins and beta-lactam antibiotics, which have bactericidal effects by disrupting the cell wall. Therefore, antibiotics like tetracycline and erythromycin are used instead. Play Video + Quiz |
 |
Klebsiella is a gram-negative, oxidase-negative bacilli with a prominent polysaccharide capsule. Infections can lead to wide range of diseases, including pneumonia and nosocomial urinary tract infections. Klebsiella pneumoniae is a form of pneumonia commonly associated with aspiration in alcoholics. People with diabetes are also more susceptible to Klebsiella infections. Patients with Klebsiella pneumoniae often cough up characteristic sputum described as red currant jelly. Severe pneumonia can also lead to lung abscesses. Besides pneumonia, Klebsiella is also associated with urinary tract infections, especially in the hospital setting. Play Video + Quiz |
 |
Pseudomonas aeruginosa is a gram-negative, aerobic bacilli that has been increasingly recognized as an opportunistic human pathogen that can cause a wide variety of infections including infections in burn patients, osteomyelitis, endocarditis, pneumonia, and urinary tract infections. P. aeruginosa most commonly infects the pulmonary tract, causing a diffuse bronchopneumonia in patients. Individuals with cystic fibrosis are especially at risk for Pseudomonas infections in the lungs. It is the most common cause of infections in burn injuries and can lead to hemorrhage and necrosis of infected tissue. It is also a common cause of hot tub folliculitis, which is caused by lack of proper, periodic attention to water quality. This organism is a frequent colonizer of medical devices including catheters and can cause nosocomial urinary tract infections. It is also frequently associated with osteomyelitis in IV drug users and also puncture wounds of the foot, thought to result from exposure to the organism via the foam padding found in tennis shoes. Diabetic patients are particularly at high risk for osteomyelitis occurring via this mechanism. This organism is implicated in corneal infections in contact lens users and can cause endocarditis when in the blood stream. Pseudomonas is also associated with purple-black skin lesions called ecthyma gangrenosum. Play Video + Quiz |
 |
Haemophilus influenzae is a gram-negative coccobacillus that can cause several diseases, including meningitis, pneumonia, otitis media, and epiglottitis. Most strains of H. influenzae live in their host without causing disease, and only cause problems when the host has reduced immune function or inflammation in the area. Naturally acquired disease can occur in infants and young children. Type b Haemophilus influenzae can cause pneumonia and bacterial meningitis. It can also cause otitis media and epiglottitis. In fact, this organism is the most common etiologic agent associated with epiglottitis, which has a thumbprint sign seen on X-ray. Ceftriaxone antibiotic is commonly used for treatment in severe cases. Play Video + Quiz |
Question 1 |
A 45 year-old male presents with sudden onset of pleuritic chest pain, productive cough and fever for 1 day. He relates having symptoms of a "cold" for the past week that suddenly became worse yesterday. Which of the following findings will most likely be seen on physical examination of this patient?
spoken "ee" heard as "ay" | |
hyperresonant percussion note Hint: Consolidation from bacterial pneumonia causes findings of dullness to percussion, late inspiratory crackles and bronchial breath sounds over the involved area. | |
wheezes over the involved area Hint: See explanation B. | |
vesicular breath sounds over involved area Hint: See explanation B. |
Question 2 |
Piperacillin Hint: Antipseudomonal penicillins, such as piperacillin, added to an aminoglycoside or fluoroquinolone are indicated for empiric treatment of nosocomial pneumonia. | |
Vancomycin Hint: Use of vancomycin should be restricted to cases where there is a high index of suspicion of involvement of methicillin resistant Staphylococcus aureus (MRSA). | |
Clindamycin Hint: Clindamycin is indicated in cases of suspected anaerobe involvement. | |
Azithromycin |
Question 3 |
Ticarcillin Hint: Infections caused by Klebsiella organisms are resistant to both ticarcillin and ampicillin. | |
Cefotaxime | |
Doxycycline Hint: See B for explanation. | |
Clindamycin Hint: See B for explanation. |
Question 4 |
tuberculosis. Hint: Most children with pulmonary tuberculosis are asymptomatic with few physical examination findings. The results of the diagnostic studies do not support tuberculosis as the most likely diagnosis. | |
mycoplasma pneumonia. | |
pneumococcal pneumonia. Hint: The clinical presentation of bacterial pneumonias in children is variable, but usually involves fever of acute onset. The WBC count is also usually elevated, making this a less likely diagnosis. | |
staphylococcal pneumonia. Hint: See C for explanation. |
Question 5 |
Administer nebulized corticosteroids Hint: Inhaled corticosteroids are not utilized in the management of community-acquired pneumonia. | |
Admit to the hospital | |
Oral antimicrobial therapy Hint: Due to the age of the patient, comorbid diseases, and current signs of respiratory distress, intravenous not oral antimicrobial therapy is indicated. | |
Endotracheal intubation Hint: Endotracheal intubation is indicated for respiratory failure unresponsive to conservative management. |
Question 6 |
Mycoplasma pneumoniae. Hint: M. pneumoniae, S. aureus, Legionella pneumophila are common pathogens for CAP, but do not account for a majority of the cases. | |
Staphylococcus aureus. Hint: See A for explanation. | |
Legionella pneumophila. Hint: See A for explanation. | |
Streptococcus pneumoniae. |
Question 7 |
Children at any age with a history of asthma Hint: Pediatric patients with cystic fibrosis, not asthma, are included in the indications for vaccination with Pneumovax, however they must be at least 2 years old. | |
All children at 2,4,6 and 12-18 months of age Hint: The 7-valent pneumococcal conjugate vaccine (Prevnar) is currently recommended to be given to children under the age of two on the schedule outlined. | |
All children at 12-23 months of age in a two dose series Hint: While a two dose series is recommended for appropriate pediatric patients that receive Pneumovax, the recommended timing between doses is 3-5 years. | |
Children age 24-59 months at high risk for invasive pneumococcal disease |
Question 8 |
Ceftriaxone (Rocephin Hint: Ceftriaxone is a third-generation cephalosporin that may be safely used in children, however is not indicated for the treatment of Chlamydial pneumonia. | |
Doxycycline Hint: Doxycycline is a tetracycline and is contraindicated in children under eight years of age secondary to damaging effects on bone and teeth enamel. | |
Levofloxacin (Levaquin) Hint: Levofloxacin is a fluoroquinolone and is contraindicated for use in children under 18 years of age secondary to damaging effects that may occur with growing cartilage. | |
Erythromycin |
Question 9 |
Resonant to percussion Hint: Physical examination findings that are consistent with a diagnosis of lobar pneumonia include dullness to percussion, increased tactile fremitus and a trachea that is midline. | |
Late inspiratory crackles | |
Decreased tactile fremitus Hint: Physical examination findings that are consistent with a diagnosis of lobar pneumonia include dullness to percussion, increased tactile fremitus and a trachea that is midline. | |
Tracheal shift toward uninvolved side Hint: Physical examination findings that are consistent with a diagnosis of lobar pneumonia include dullness to percussion, increased tactile fremitus and a trachea that is midline. |
Question 10 |
Nafcillin Hint: Nafcillin is classified as a penicillinase-resistant penicillin, however would not be effective against methicillin- resistant strains of Staphylococcus aureus. | |
Vancomycin | |
Clindamycin Hint: Clindamycin is primarily utilized in treatment of severe anaerobic infections, but is not indicated for the treatment of methicillin-resistant Staphylococcus aureus. | |
Doxycycline Hint: Doxycycline is a tetracycline and is only utilized to treat respiratory infections that are susceptible to tetracycline, such as Mycoplasma or Chlamydial pneumonias. |
Question 11 |
Decreased red blood cells Hint: The presence or absence of red blood cells is not a criterion for determining the adequacy of a sputum sample. | |
Decreased bronchial epithelial cells Hint: The presence of bronchial epithelial cells confirms the sample came from the lower respiratory tract. | |
Increased Gram positive cocci Hint: The presence of Gram positive cocci has no bearing on the adequacy of the sputum sample. | |
Increased polymorphonuclear leukocytes |
Question 12 |
IV drug abuse | |
Alcohol abuse Hint: A history of alcohol abuse is commonly seen with pneumonia caused by Klebsiella pneumoniae. | |
Poor dental hygiene Hint: Poor dental hygiene is associated with pneumonia caused by anaerobes. | |
HIV positive patient Hint: HIV positive patients are most at risk for development of pneumonia caused by Pneumocystis jiroveci. |
Question 13 |
Respiratory syncytial virus Hint: RSV is characterized by wheezing on auscultation and the course is typically 3-7 days. | |
Influenza virus Hint: Influenza pneumonia is characterized by a more precipitous onset and fulminant course. | |
Mycoplasma pneumoniae | |
Streptococcus pneumoniae Hint: Pneumococcal pneumonia is typically characterized by a more severe illness and more fulminant course. |
Question 14 |
Lobar consolidation Hint: Lobar consolidation is seen in community-acquired pneumonia. | |
Apical infiltration Hint: Apical infiltration is seen in tuberculosis. | |
Granulomatous inflammation Hint: Granulomatous inflammation is seen in sarcoidosis. | |
Diffuse nodular densities |
Question 15 |
Decreased tactile fremitus Hint: Consolidation would increase the transmission of vocal vibrations and manifest as increased tactile fremitus. | |
Egophony | |
Hyperresonance to percussion Hint: Dullness, not hyperresonance, would be expected with consolidation. | |
Wheeze Hint: Wheezing is associated with narrowing of the small airways as seen in asthma. |
Question 16 |
Legionella | |
Chlamydophila Hint: Chlamydophila pneumonia is associated with dry cough, low-grade fever, and hoarseness. | |
Mycoplasma Hint: Mycoplasma pneumonia is most likely complicated by bullous myringitis, hoarseness, rash, and chronic cough. | |
Pneumococcal Hint: Pneumococcal pneumonia presents with a single rigor, rust-colored sputum, and productive cough. There is no diarrhea as part of its infection. |
Question 17 |
Hyperresonance Hint: Hyperresonance is an abnormal sound as a result of air trapping as in COPD. | |
Vesicular breath sounds Hint: Vesicular breath sounds are the description of normal lung sounds. | |
Increased tactile fremitus | |
Wheezing Hint: Wheezing is a musical noise sounding like a squeak caused by high velocity air flow through a narrow or obstructed airway. |
|
List |
References: Merck Manual · UpToDate · EMRA antibiotic guide


 Lecture
Lecture



