Pulmonary Circulation (PEARLS)
The NCCPA™ PANCE Pulmonary Content Blueprint addresses three types of pulmonary circulation disorders
| Cor pulmonale |
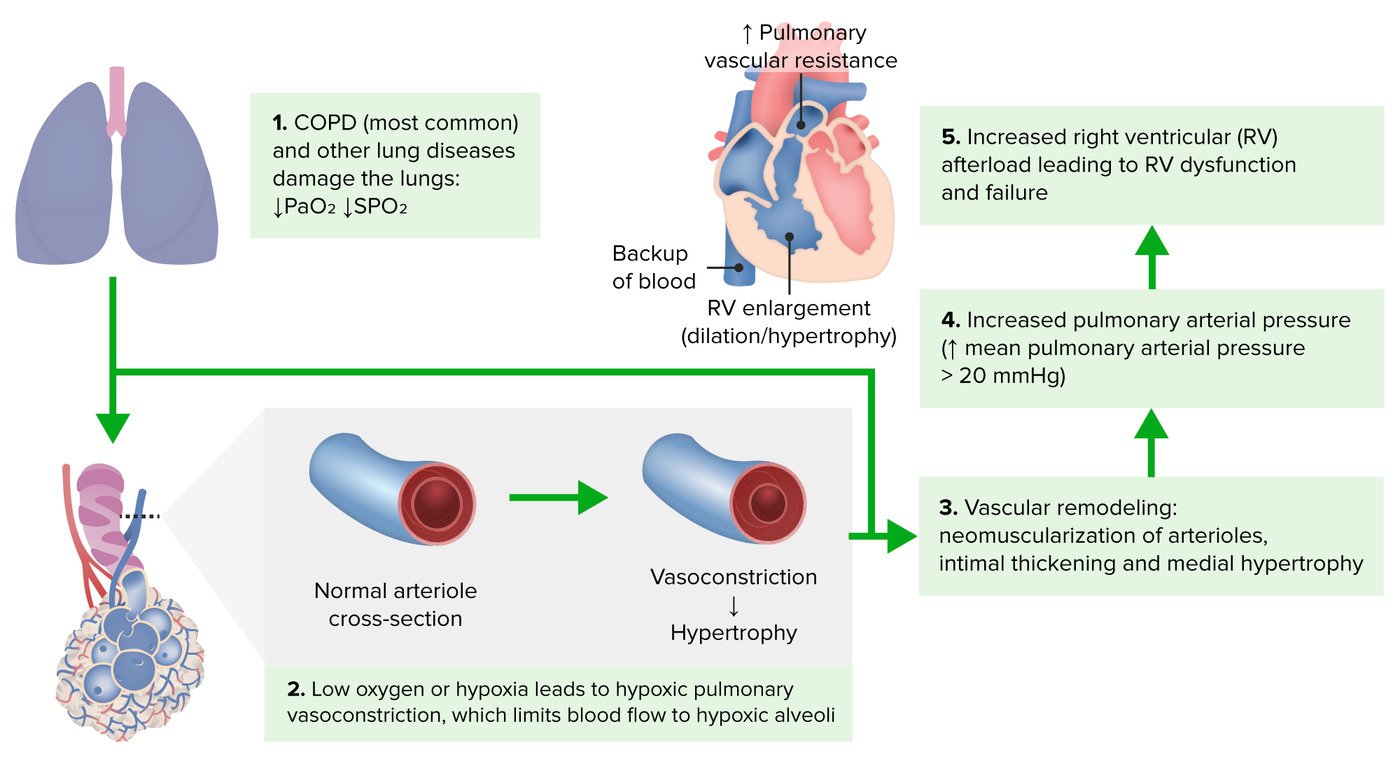
Patient will present as → 65 y/o with 3 days of progressive dyspnea and purulent sputum production. The patient takes albuterol and tiotropium bromide for moderate COPD. His PMH is relevant for a 40-pack-year smoking history, type II DM, hyperlipidemia, and coronary artery stenting 2 years ago. Physical exam shows a barrel-shaped chest, inspiratory crackles, hepatojugular reflux, pulsus paradoxus, and ventricular gallop. His temperature is 100.3°F, his pulse is 130/min, respirations are 28/min, blood pressure is 130/84 mmHg, and pulse oximetry on room air shows an oxygen saturation of 86%. Right ventricular enlargement and eventually failure secondary to lung disorder that causes pulmonary artery HTN
- Etiology: COPD (most common), pulmonary embolism, vasculitis, asthma, ILD, acute respiratory distress syndrome
- Physical Exam: Lower extremity edema, neck vein distention, hepatomegaly, parasternal lift, tricuspid/pulmonic insufficiency, loud S2
DX: The diagnosis of cor pulmonale is usually made with an echocardiogram → increased pressure in the pulmonary arteries and right ventricle
- Spirometry can be done to look for chronic lung disease
- The gold standard diagnostic test to directly measure pulmonary pressures and assess for response to vasodilating medications is a right heart catheterization
TX: Diagnose and treat the underlying condition before cardiac structure change becomes irreversible
-
- Diuretics are not helpful and may be harmful!
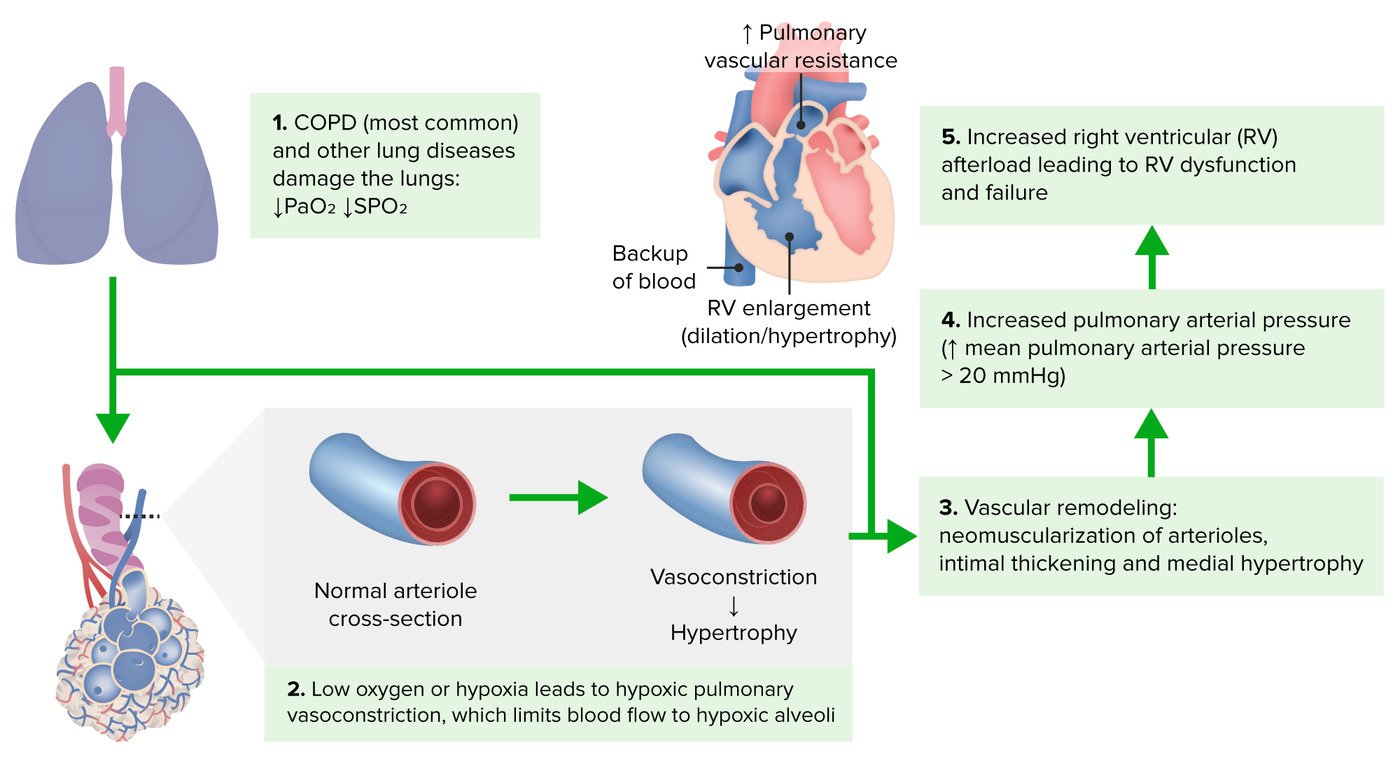 Pathophysiology of cor pulmonale (Image by Lecturio) |
| Pulmonary embolism (ReelDx) |
Patient will present as → 68 y/o F who underwent hip replacement surgery two weeks ago. The postoperative period was complicated by pneumonia, and the patient has been bedridden ever since. A nurse calls you to the patient’s room due to vital sign abnormalities and complaints of chest pain. The patient’s HR is 105 bpm, BP is 90/60 mmHg, RR is 35 rpm, and T is 100.2F. You note jugular venous distension and profound dyspnea. Upon auscultation, you notice tachypnea and crackles. pulmonary embolism

You are called to see a 51 y/o male with an acute onset of shortness of breath x 24 hours
- Gender: Male
- Age: 51 years
- Weight: 253.5 lb/115 kg
- Height: 73 in/185.4 cm
- Temperature: 97.7 F/36.5 C
- Blood Pressure: 139/98
- Heart Rate: 113
- Respiratory Rate: 20
- Pulse Oximetry: 96% RA
- Acute onset of shortness of breath the previous night
Click here to work through this patient case simulation.
A pulmonary embolism is a blockage in one of the pulmonary arteries in the lungs
- More than 90% originate from clots in the deep veins of the lower extremities
- Presents with dyspnea (most common) and pleuritic chest pain
- R/F: Virchow’s triad = hypercoagulable state, trauma, venostasis (surgery, cancer, oral contraceptives, pregnancy, smoking long bone fracture/fat emboli)
- Homan’s sign: (Dorsiflexion of the foot causes pain in calf) indicative of deep vein thrombosis
- EKG: TACHYCARDIA (most common), S1Q3T3 (rare), non-specific ST wave changes
Diagnosis: Well’s Score is used to assess the probability of pulmonary embolism
- Spiral CT = initial method of identifying
- Pulmonary angiography = gold standard definitive
- CXR: Westermark sign or Hampton hump (triangular or rounded pleural base infiltrate adjacent to hilum)
- VQ scans are "old school"= perfusion defects with normal ventilation (normal VQ rules out PE; abnormal – non-specific)
- Venous duplex ultrasound of lower extremities (normal test does not exclude PE)
- ABG = respiratory alkalosis secondary to hyperventilation
- D-dimer
Tx: Heparin is the anticoagulant of choice for the acute phase with factor Xa inhibitors (e.g., rivaroxaban, apixaban, edoxaban) and oral direct thrombin inhibitors (dabigatran) thereafter

|
| Pulmonary hypertension |
Patient will present as → 43 y/o F with a history of COPD presents to the office with worsening dyspnea, especially at rest. She also complains of dull, retrosternal chest pain. On examination, she has persistent widened splitting of S2. Radiographic findings ( seen here) demonstrate peripheral “pruning” of the large pulmonary arteries. Blood pressure in the lungs is usually extremely low 15/5. In pulmonary hypertension, the pressure increases > 20 mmHg at rest
- Usually caused by an underlying disorder (constrictive pericarditis, mitral stenosis = MC, LV failure, mediastinal disease compression pulmonary veins)
- Mitral stenosis: mitral valve = tight so blood can’t pass into left ventricle ⇒ pressure backs up to lungs
- When the right heart can’t pump against vascular resistance ⇒ right heart failure = Cor pulmonale
- Presentation: Dyspnea on exertion, fatigue, chest pain, edema
- Physical Exam: Loud pulmonic component of second heart sound (P2); Jugular venous distension; Ascites; Hepatojugular reflux; Lower limb edema
Diagnose with a right heart catheterization (gold standard) → most accurate measure of pressures
- CXR
- Enlarged pulmonary arteries
- Lung fields may or may not be clear, dependent on the underlying cause
- Echocardiogram
- Increased pressure in pulmonary arteries, right ventricles → dilated pulmonary artery
- Dilatation/hypertrophy of right atrium, right ventricle
- Large right ventricle → bulging septum
- ECG → Right heart strain pattern: T wave inversion in right precordial (V1–V4) and inferior leads (II, III, aVF)
TX: identify and treat the underlying cause
- Pulmonary hypertension secondary to left ventricular failure → optimize left ventricular function
- Diuretics (cautiously—individuals may be preload dependent)
- Digoxin
- Anticoagulants
- Cardiogenic pulmonary arterial hypertension
- Relax smooth muscle (promote vasodilation), reduce vascular remodeling, improve exercise capacity with prostanoids, phosphodiesterase inhibitors, endothelin antagonists
- Pulmonary arterial hypertension
- Endothelin receptor antagonists
- Prostanoids
 The classic findings on chest radiography in a patient with pulmonary arterial hypertension include enlarged central pulmonary arteries that taper distally (peripheral pruning), attenuated peripheral vessels, and oligemic lung fields. |
Back to PANCE Blueprint Pulmonary (10%)