Patient will present as → a patient brought to the emergency room with acute onset of dyspnea and tachypnea. He has a long history of alcoholism and was involved in a motor vehicle accident two days ago. He is hypoxic with crackles auscultated bilaterally and frothy pink sputum. Chest radiography reveals diffuse bilateral infiltrates, which spare the costophrenic angle and air bronchograms. There is no cardiomegaly or pleural effusion noted. Oxygen saturation is 70%.
To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
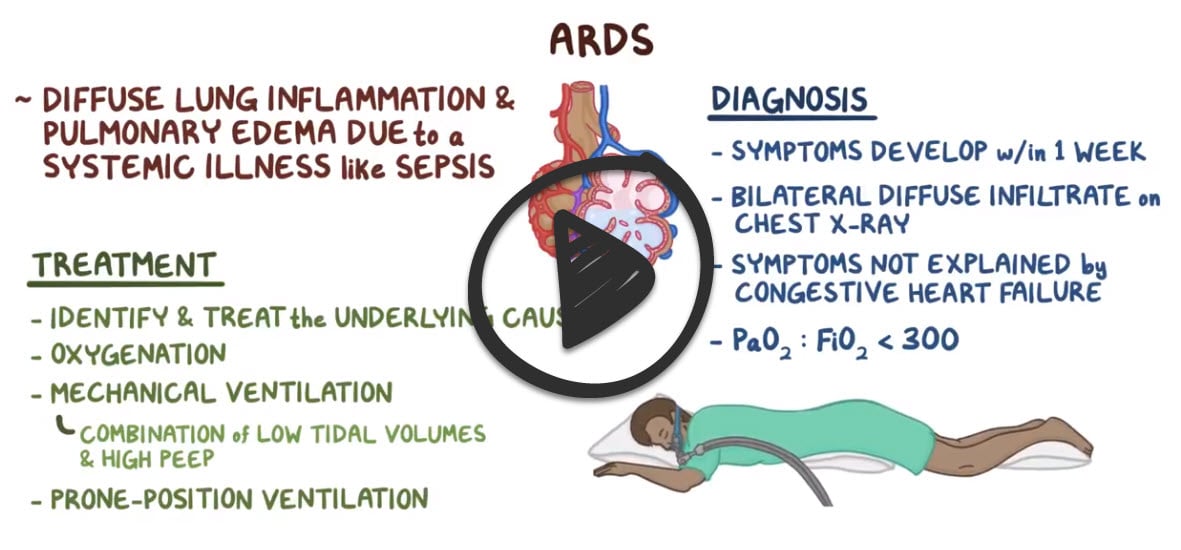
Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by fluid collecting in the lungs, depriving organs of oxygen
- The underlying abnormality in ARDS is ⇑ permeability of alveolar-capillary membranes ⇒ development of protein-rich pulmonary edema (non-cardiogenic pulmonary edema)
- ARDS can occur in those who are critically ill or who have significant injuries
Three clinical settings account for 75% of ARDS cases:
- Sepsis syndrome (most common cause)
- Severe multiple trauma
- Aspiration of gastric contents (alcoholics), toxic inhalation, near-drowning
People with ARDS have severe shortness of breath and often are unable to breathe on their own without support from a ventilator
- Rapid onset of profound dyspnea occurring 12-24 hours after the precipitating event
- Tachypnea, pink frothy sputum, crackles
- Hyaline membrane disease/respiratory distress syndrome in preterm infants (RDS) is often due to young gestational age, immature type II alveolar cells, and lack of alveolar surfactant, resulting in inadequate alveolar surface tension during expansion, which results in atelectasis, reduced gas exchange, severe hypoxia, and acidosis.
- Hyaline membrane disease and RDS are two names for the same thing!
- Acute respiratory distress syndrome (ARDS) in newborns and children is distinct from RDS/Hyaline membrane disease and involves diagnostic criteria (Montreux standard). Unlike RDS, ARDS of newborns and children is not based on a lack of alveolar surfactant.
- These diagnostic criteria for ARDS of newborns and children include:
- Acute exacerbation (within 1 week) after clinical or possible injury
- Not caused by RDS, transient tachypnea of the newborn (TTN), congenital malformations, atelectasis, local effusions
- Congenital heart disease that can be explained by pulmonary edema
- Oxygenation index (OI) value ≥4
- Chest radiograph shows air bronchograms and bilaterally fluffy infiltrate
- Normal BNP, pulmonary wedge pressure, left ventricle function, and echocardiogram
Treatment involves identifying and managing underlying precipitation and secondary conditions
- Tracheal intubation with the lowest level PEEP to maintain PaO2 > 60 mmHg or SaO2 > 90
- ARDS is often fatal. The risk increases with age and the severity of illness
 Osmosis Osmosis |
|
 |
ARDS is a sudden and progressive failure of the respiratory system in which the alveolar-capillary membrane becomes damaged. Damage to this membrane makes it more permeable to fluid, which can lead to difficulty breathing, atelectasis, and hypoxemia that is unresponsive to oxygen therapy. Patients who develop ARDS are typically afflicted by another illness or injury such as COPD, pneumonia, tuberculosis, aspiration, sepsis, shock, or fluid overload. Patients with this condition may also develop pulmonary hypertension, which is a late indicator of decreased lung compliance.
Play Video + QuizAcute Respiratory Distress Syndrome (ARDS) Interventions
Patients with ARDS are at an increased risk for developing renal failure and stress ulcers. Close monitoring of patients for these conditions is essential. Hemodynamic monitoring should also be an important component of care, as these patients may experience hypotension, hypoxemia, and hypercapnia, which can cause negative consequences if left untreated.
Play Video + QuizNeonatal respiratory distress syndrome (NRDS)
Neonatal respiratory distress syndrome (NRDS) is a condition related to fetal lung immaturity in premature infants (<37 weeks gestational age) and a lack of surfactant. Infants with NRDS will exhibit signs of respiratory distress including tachypnea, nasal flaring, intercostal/substernal retractions, and audible grunting upon expiration. Interventions used to treat NRDS include administration of exogenous surfactant, oxygen therapy, and mechanical ventilation. It is important to note that infants with NRDS should not receive bottle or gavage feedings, as these may increase their respiratory rate and risk of aspiration. Instead, total parenteral nutrition (TPN) is used to provide the infant with adequate nutrients.
Play Video + QuizQuestion 1 |
Atelectasis Hint: Small areas of atelectasis usually are asymptomatic. While larger areas may present with similar clinical findings, the chest x-ray findings are not consistent with atelectasis. | |
Diaphragmatic hernia Hint: Chest x-ray in a patient with a diaphragmatic hernia would not show a fine reticular granular pattern. | |
Respiratory distress syndrome | |
Pneumothorax Hint: Chest x-ray in a patient with a pneumothorax would not show a fine reticular granular pattern. |
Question 2 |
Tracheal intubation | |
Bilateral chest tube insertion Hint: Chest tube insertion is not indicated in a patient with ARDS. | |
Type-specific packed cells Hint: Fluids are the preferred treatment initially for hypovolemia. Type-specific packed cells are given when the patient's blood type is identified. Until then O negative packed cells are administered. | |
Colloid solutions Hint: Use of crystalloid solutions are preferred to avoid pulmonary edema. | |
Provide supplemental oxygen Hint: Marked hypoxemia is refractory to treatment with supplemental oxygen in ARDS. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture