9-year-old with right-sided ear pain x 1 day
9-year-old with right-sided ear pain x 1 day
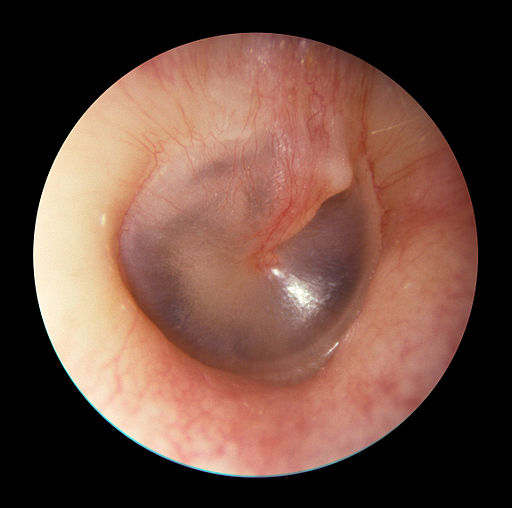
Patient will present as → a 9-year-old female with right otalgia and a nonproductive cough for one day. The patient complains of constant popping in her ears and fluctuating conductive hearing loss with tinnitus. The patient has no significant past medical history, her immunizations are up to date, and both of her parents are non-smokers. On otoscopic examination, the tympanic membranes are grey with normal landmarks, including visualization of the middle ear ossicles. There is no evidence of bulging pus or exudate suggestive of an acute inflammatory process.
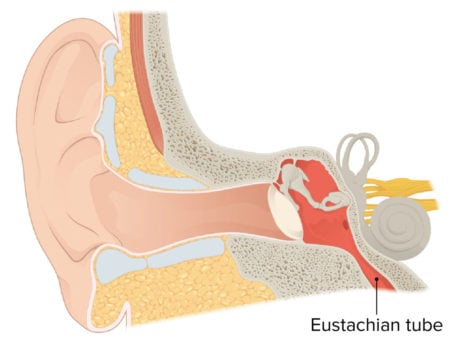
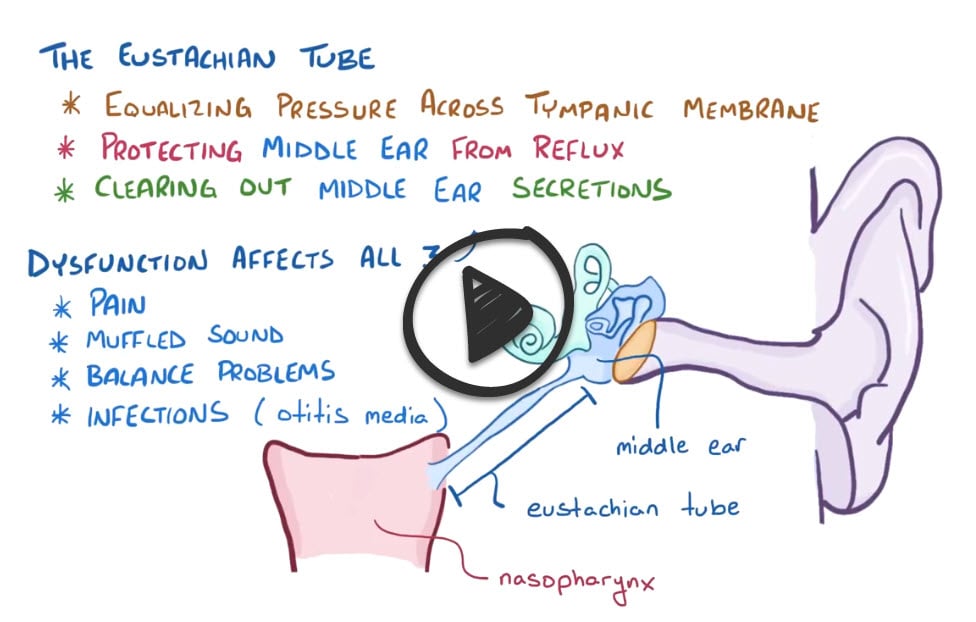
The eustachian tube connects the middle ear to the nasopharynx and is useful for equalizing pressure across the tympanic membrane, protecting the middle ear from reflux, and clearing out middle ear secretions
- Eustachian tube dysfunction (ETD) is defined as a failure of the functional valve of the eustachian tube to open and/or close properly
- ETD usually follows the onset of an upper respiratory infection
- Will present with ear fullness, popping of ears, underwater feeling, intermittent sharp ear pain, fluctuating conductive hearing loss, and tinnitus
- Eustachian tube dysfunction is a primary cause of acute otitis media (AOM) and otitis media with effusion (OME)
- All children < 7 years old have some ET dysfunction
An excellent otoscopic exam is the key to making this diagnosis – otoscopic findings are usually normal. May see fluid behind TM if acute serous otitis media
- The definitive diagnosis is with a tympanogram
- In cases of persistent effusion, CT or MRI may be indicated (neoplasm may cause eustachian tube obstruction)
All children < 7 years old have some ET dysfunction (based on the angle of the Eustachian tube) that will resolve with age
- Ibuprofen as needed for pain
- Nasal steroids can be prescribed in more severe cases
- Systemic decongestants, such as pseudoephedrine or phenylephrine, may be helpful for nasal congestive symptoms
- Surgery (tympanostomy tubes) is generally indicated when medical management fails
Question 1 |
Acute otitis media Hint: Typically presents with ear pain and possibly fever. | |
Chronic otitis externa Hint: Involves the external ear canal, often with itching and discharge. | |
Meniere's disease Hint: Characterized by episodic vertigo, tinnitus, and fluctuating hearing loss. | |
Eustachian tube dysfunction | |
Vestibular schwannoma Hint: Presents with unilateral hearing loss and tinnitus, not typically affected by pressure changes. |
Question 2 |
Feeling of fullness in the ear Hint: This is a common symptom of Eustachian tube dysfunction, as the tube's inability to properly equalize pressure can lead to a sensation of fullness or blockage. | |
Tinnitus Hint: Eustachian tube dysfunction can cause tinnitus, or ringing in the ear, due to pressure changes or fluid accumulation in the middle ear. | |
Vertigo | |
Muffled or diminished hearing Hint: This can occur in Eustachian tube dysfunction as a result of fluid accumulation or negative pressure in the middle ear, affecting sound conduction. | |
Otalgia (ear pain) Hint: Ear pain or discomfort can be a symptom of Eustachian tube dysfunction, often due to pressure changes or fluid buildup in the middle ear. |
Question 3 |
Tympanometry | |
Pure-tone audiometry Hint: While useful for assessing the degree and type of hearing loss, pure-tone audiometry does not specifically diagnose middle ear effusion. | |
High-resolution computed tomography (CT) of the temporal bone Hint: This imaging modality is more appropriate for detailed assessment of bony structures and is typically reserved for cases where there is suspicion of more complex pathology than effusion. | |
Magnetic resonance imaging (MRI) of the brain Hint: MRI is not the first-line diagnostic tool for middle ear effusion as it is more suited for evaluating central nervous system pathology. | |
Otoscopic examination Hint: While otoscopy can visualize the tympanic membrane and provide some information about effusion, tympanometry is more definitive for evaluating the functional impact of the effusion on the middle ear. |
Question 4 |
Systemic decongestants and nasal corticosteroids | |
Antibiotic therapy Hint: Indicated if there is evidence of concurrent bacterial infection. | |
Surgical intervention with tympanostomy tubes Hint: Considered in chronic or severe cases unresponsive to medical therapy. | |
Hearing aids Hint: Used for significant hearing loss, which is not the primary issue in Eustachian tube dysfunction. | |
Vestibular rehabilitation exercises Hint: More appropriate for disorders affecting balance and vestibular function. |
|
List |
References: Merck Manual · UpToDate


 Osmosis
Osmosis