Patient with open-angle glaucoma presents as → a 47-year-old African American male presents for an ophthalmic examination. Medical history is significant for hypertension and type II diabetes mellitus. On slit-lamp examination, there is cupping of the optic disc, with a cup-to-disc ratio > 0.6. Tonometry reveals intraocular pressure of 45 mmHg (normal is 8-21 mmHg). Peripheral field vision loss is noted on the visual field exam.
Patient with acute angle closure glaucoma will present with → a 60-year-old Asian American woman presents with sudden ocular pain. She reports she was visiting the planetarium when the pain started, and when she walked outside, she saw halos around the street lights. The pain was so bad that she began to vomit. She reports her vision is decreased. Physical examination reveals conjunctival injection, a cloudy cornea, and a fixed dilated pupil.
To watch this and all of Joe Gilboy PA-C's video lessons, you must be a member. Members can log in here or join now.
Open-angle Glaucoma
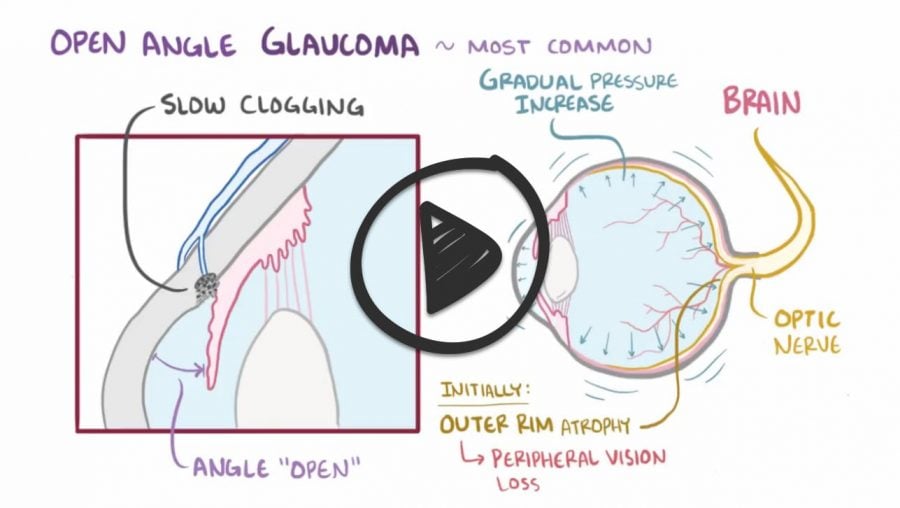
- Impaired aqueous outflow through a diseased trabecular meshwork causing increasing IOP, leading to a gradual increase in pressure and progressive peripheral visual field loss
- Open-angle glaucoma is the most common type, accounting for 90% of glaucomas in the US
- Open-angle glaucoma is also more common to occur in one eye at first, but it is more likely to affect both eyes over time.
- Pt will likely be African American and be asymptomatic – diagnosed during routine screening. This is an insidious, slow process – pt will usually be unaware
- Visual loss in open-angle progresses from peripheral → central = glaucoma
- Visual loss from central → peripheral = macular degeneration
Acute angle closure glaucoma (ophthalmologic emergency)
- Occurs when the iris dilates and pushes against the lens of the eyes, disrupting the flow of aqueous humor into the anterior chamber. The pressure in the posterior chamber then pushes the peripheral iris forward and blocks the angle
- Acute and severe pain, unilateral, decreased visual acuity with headache, nausea and vomiting
- Classic triad of injected conjunctiva, cloudy cornea, and fixed dilated pupil
| Feature | Acute angle-closure glaucoma | Open-angle glaucoma |
|---|---|---|
| Definition | A medical emergency that occurs when the iris blocks the drainage angle of the eye, causing a sudden and severe increase in intraocular pressure (IOP). | A chronic eye condition that damages the optic nerve and can lead to vision loss. |
| Symptoms | Severe eye pain, redness, blurry vision, headache, nausea, vomiting. | May have no symptoms in the early stages. As the disease progresses, symptoms may include blurred vision, gradual loss of peripheral vision, and difficulty seeing in low light. |
| Risk factors | Narrow anterior chamber angle, hyperopia (farsightedness), family history of glaucoma, age over 40, Asian descent. | Age over 40, family history of glaucoma, African American or Hispanic descent, high blood pressure, diabetes, and certain medications. |
| Onset | Sudden | Gradual |
| IOP | IOP typically exceeds 40 mm Hg. | IOP is typically within the normal range (10-21 mm Hg), but can be elevated, especially in advanced stages of the disease. |
| Treatment | Immediate medical attention is required to lower IOP and prevent vision loss. Treatment may include laser iridotomy, iridectomy, and/or medications. | Medications are typically the first-line treatment for open-angle glaucoma. Surgery may be considered if medications are not effective. |
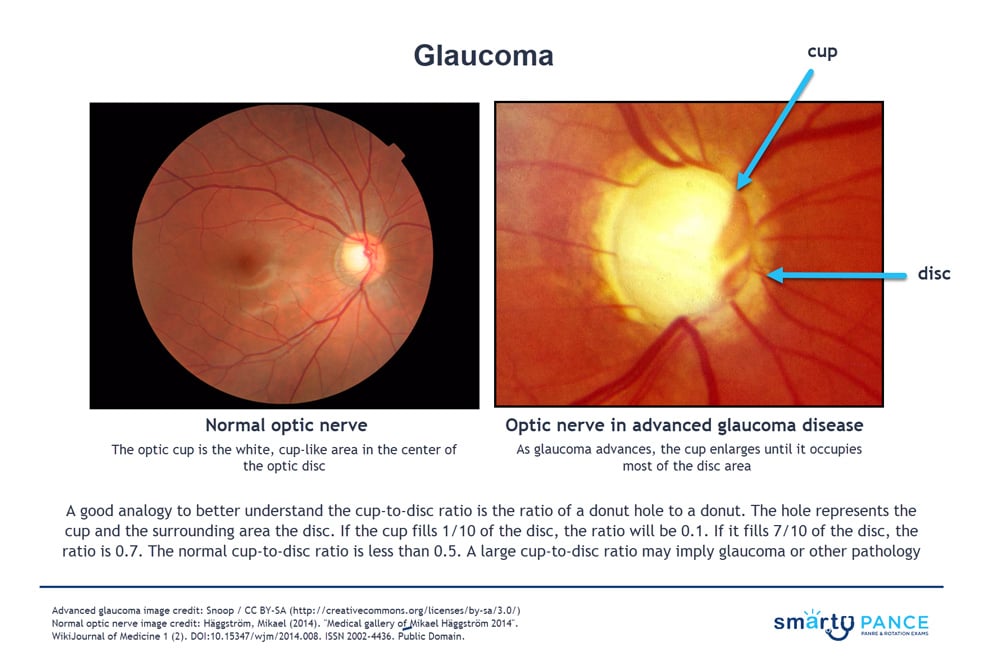
Diagnosis is confirmed by tonometry demonstrating increased intraocular pressure
- May demonstrate cupping of the optic nerve
All patients should be screened at age 40 - may present for routine fundoscopy with a cup-to-disk ratio > 0.5 (<0.5 is normal). This is suggestive but not diagnostic of glaucoma, so you will progress to the next step, which is tonometry
- Perform tonometry (IOP testing): pressure > 21 mmHg is concerning but not diagnostic - proceed to the next step, which is peripheral field testing
- Peripheral field testing and optic disc changes confirm the diagnosis in normal pressure glaucoma
- Gonioscopy is the gold-standard method of diagnosing angle-closure glaucoma. This technique involves using a special lens for the slit lamp, which allows the ophthalmologist to visualize the angle
Acute Narrow-Angle Closure Glaucoma
- IV Acetazolamide: the first-line agent - decrease IOP by decreasing aqueous humor production
- Topical beta-blockers (e.g. timolol) reduce IOP without affecting visual acuity
- Miotics/cholinergics (e.g. Pilocarpine, Carbachol)
- Peripheral iridotomy (punches a hole in the iris) is the definitive treatment
Chronic Open-Angle Glaucoma
- Prostaglandin analogs are 1st line (ex. latanoprost) - increases the outflow of aqueous humor
- Topical beta-blocker (Timolol) - decrease production of aqueous humor
- Trabeculoplasty - opens the trabecular meshwork
 Osmosis Osmosis |
|
 |
 With all types of glaucoma, the nerve connecting the eye to the brain is damaged, usually due to high eye pressure. The most common type of glaucoma (open-angle glaucoma) often has no symptoms other than slow vision loss. Angle-closure glaucoma, although rare, is a medical emergency and its symptoms include eye pain with nausea and sudden visual disturbance. Treatment includes eye drops, medications, and surgery.
With all types of glaucoma, the nerve connecting the eye to the brain is damaged, usually due to high eye pressure. The most common type of glaucoma (open-angle glaucoma) often has no symptoms other than slow vision loss. Angle-closure glaucoma, although rare, is a medical emergency and its symptoms include eye pain with nausea and sudden visual disturbance. Treatment includes eye drops, medications, and surgery.
| Open-angle glaucoma | Play Video + Quiz |
| Closed-angle glaucoma | Play Video + Quiz |
| Acetazolamide | Play Video + Quiz |
| Pilocarpine | Play Video + Quiz |
Question 1 |
Migraine headache Hint: Migraine headache does not present with eye findings. | |
Temporal arteritis Hint: Temporal arteritis presents with headache and systemic symptoms of fever, myalgias, anorexia, and tenderness over the temporal artery. | |
Acute glaucoma | |
Retinal artery occlusion Hint: Retinal artery occlusion presents with sudden, painless, severe loss of vision. There are no systemic symptoms. |
Question 2 |
Cortical blindness Hint: Cortical blindness is a rare adverse effect when prescribing salicylates. | |
Optic atrophy Hint: Optic atrophy can occur as an adverse effect with lead compounds, amebicides, and MAO inhibitors. | |
Glaucoma | |
Papilledema Hint: Papilledema can be a side effect to many systemic medications. |
Question 3 |
metoclopramide | |
timolol Hint: Timolol, a beta-antagonist, is used in the treatment of acute angle-closure glaucoma. | |
glyburide Hint: Glyburide has no relationship to glaucoma. | |
acetazolamide Hint: Acetazolamide, a carbonic anhydrase inhibitor, may suppress the production of aqueous humor by 40-60% and is used in the emergency treatment of glaucoma. |
Question 4 |
Acute glaucoma | |
Migraine Hint: Migraine headaches have associated unilateral headache and nausea however there would be no pupillary changes. | |
Episcleritis Hint: Episcleritis is an inflammation of the thin layer of connective tissue between the conjunctiva and sclera. Episcleritis resembles conjunctivitis but is a more localized process and discharge is absent. | |
Acute uveitis Hint: Acute uveitis is frequently due to systemic disorders associated HLA-B27-related conditions ankylosing spondylitis, reactive arthritis, psoriasis, ulcerative colitis, and Crohn's disease. The pupil is usually small, inflammatory cells and flare within the aqueous are present. |
Question 5 |
Contact lens use Hint: The major risk from contact lens wear is bacterial, amebic, or fungal corneal infection, potentially a blinding condition. In this condition the eye may appear red, however the cornea would be clear, and the globe would not be tense. | |
Past sexual contacts Hint: Past sexual contacts would be related to pupillary abnormalities associated with neurosyphilis. | |
Recent URI symptoms Hint: URI symptoms would be considered when associated with conjunctivitis. Pupil size is normal and is the pupillary light response. Intraocular pressure is normal. | |
Visualizing halos around street lights |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture