
24 y/o with fever and right-sided sinus pain
Patient will present as → a 34-year-old previously healthy male with complaints of facial pressure and rhinorrhea for the past 3 weeks. The patient reports that several weeks prior, he had a “common cold,” which resolved. However, he has since developed worsening facial pressure, especially over his cheeks and forehead. He reports over 1 week of green-tinged rhinorrhea. His temperature is 100.1 F (37.8 C), blood pressure is 120/70 mmHg, pulse is 85/min, and respirations are 15/min. The nasal exam reveals edematous turbinates and purulent discharge. The patient has facial tenderness with palpation over the involved sinus.
To watch this and all of Joe Gilboy PA-C's video lessons, you must be a member. Members can log in here or join now.
Looking for symptoms that worsen over 5-7 days or do not improve in > 10 days
- Symptoms: fever, facial pain, a headache that can radiate to the upper teeth, purulent rhinorrhea, congestion, and loss of smell
- Physical exam: Classically, facial tenderness with palpation over the involved sinus
Acute sinusitis
- < 4 weeks duration
- Sudden onset
- Most commonly caused by S. pneumoniae, H. influenzae, Moraxella catarrhalis
- Usually precipitated by an acute viral respiratory tract infection which is thought to lead to reduced clearance of mucus
Chronic sinusitis
- > 12 consecutive weeks
- Associated bacteria include S. aureus, anaerobes, and gram-negative organisms such as Pseudomonas aeruginosa
- Other risks include systemic disease, anatomic anomalies, trauma, noxious chemicals such as pollutants or smoke, and medications
The disease is subacute when symptomatic for 4–12 weeks and chronic when symptomatic for >12 weeks.
Plainview X-ray (Waters' view) has fallen out of favor due to poor sensitivity
- Sinus CT is the GOLD STANDARD
Diagnosis of acute bacterial rhinosinusitis (ARBS):
- ABRS should be diagnosed when signs and symptoms of acute rhinosinusitis (ARS) (purulent nasal drainage plus nasal obstruction, facial pain-pressure or both) persist without improvement for at least 10 days OR if signs and symptoms worsen within 10 days after initial improvement.
Diagnosis of chronic sinusitis:
- Chronic rhinosinusitis is characterized by 12 weeks or more of at least two of four cardinal symptoms: nasal obstruction, anterior or posterior nasal discharge, reduction or loss of smell, and facial pain/pressure/fullness.
- In addition, there must be objective evidence of mucosal inflammation, either by direct visualization or on an imaging study (usually sinus computed tomography [CT] scan)
- Duration of symptoms >10 days without improvement
- Fever greater than 102 F and/or purulent nasal discharge
- Rapid worsening of symptoms after initial improvement
First-line therapies for bacterial sinusitis in adults include (treat for 5–7 days in adults)
- Amoxicillin 500 mg orally three times daily or 875 mg orally twice daily (for patients without risk factors for pneumococcal resistance )
- Amoxicillin-clavulanate (Augmentin) 500 mg/125 mg orally three times daily or 875 mg/125 mg orally twice daily
Penicillin allergic
- Doxycycline 100 mg orally twice daily or 200 mg orally daily
- Cephalosporin (cefixime 400 mg daily or cefpodoxime 200 mg twice daily) prescribed with or without clindamycin (300 mg every six hours)
Second-line therapy (for those who fail to improve within 7 days) includes high-dose Augmentin (2 g BID x 7 days), Moxifloxacin, Levofloxacin, or a third-generation cephalosporin plus clindamycin. If improvement is seen within 7 days of initiation of therapy, antibiotic treatment should be continued for a total course of 7 to 10 days.
- Amoxicillin-clavulanate 2 g/125 mg extended-release tablets orally twice daily
- Levofloxacin 500 or 750 mg orally once daily
- Moxifloxacin 400 mg orally once daily
For penicillin-allergic patients, options include:
- Doxycycline 100 mg orally twice daily or 200 mg orally daily
- Levofloxacin 500 or 750 mg orally once daily
- Moxifloxacin 400 mg orally once daily
Chronic rhinosinusitis (CRS) lasts 12 weeks or longer despite attempts at medical management. Therapy is typically given for at least three weeks and may be extended for up to ten weeks in refractory cases
- Amoxicillin-clavulanate: 875 mg twice daily or two 1000 mg extended-release tablets twice daily
- Pen allergic: Clindamycin 300 mg four times daily or 450 mg three times daily
Children first-line is Amoxicillin-clavulanate 45 mg/kg per day in 2 divided doses if uncomplicated acute bacterial sinusitis
- Treat for 10–14 days in children if uncomplicated bacterial rhinosinusitis
- Third-generation cephalosporin (e.g., cefpodoxime or cefdinir) in children with penicillin allergy
- If there is no improvement after 72 hours, switch to a second-line agent
 Osmosis Osmosis |
|
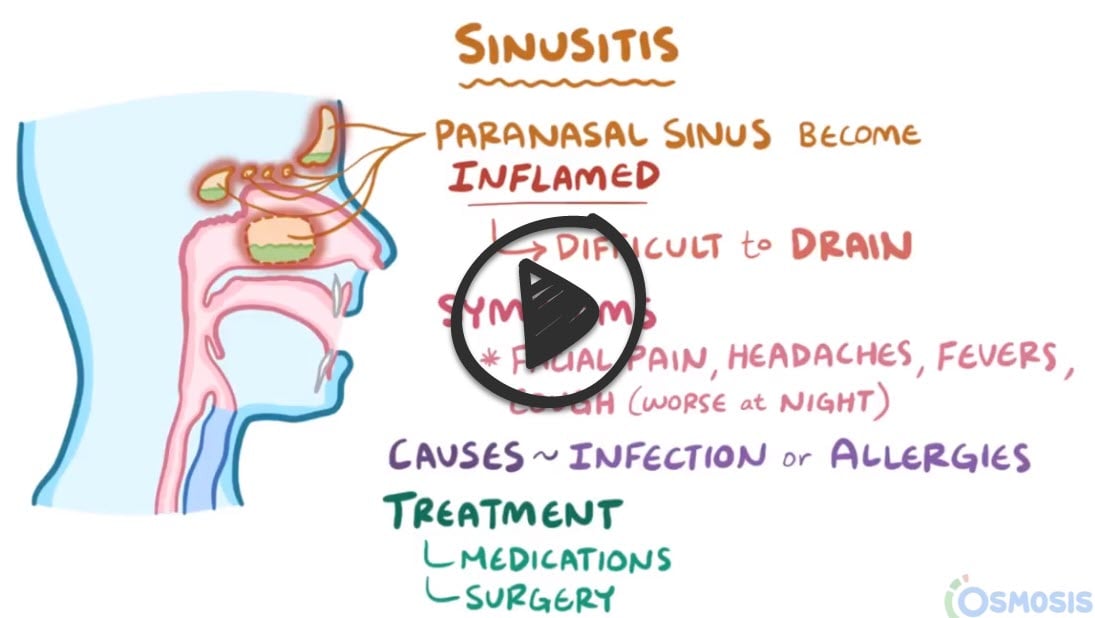 |
 Rhinosinusitis is the inflammation of the sinuses. It’s usually preceded by an upper respiratory infection. Diagnosis is usually based on symptoms including nasal drainage, facial pain, retroorbital pain, or a fever if worsening.
Rhinosinusitis is the inflammation of the sinuses. It’s usually preceded by an upper respiratory infection. Diagnosis is usually based on symptoms including nasal drainage, facial pain, retroorbital pain, or a fever if worsening.
| Rhinosinusitis assessment | Play Video + Quiz |
| Beta lactamase inhibitors | Play Video + Quiz |
| Cephalosporins | Play Video + Quiz |
Question 1 |
Duration and time course of compatible symptoms | |
Presence of purulent nasal discharge Hint: While purulent discharge can be present in ABRS, it's also seen in viral infections and isn't reliable for distinguishing the two. | |
Response to nasal decongestants Hint: Symptom improvement with decongestants can occur in both viral and bacterial sinusitis. It doesn't help differentiate between the two. | |
Severity of facial pain and fever Hint: Both ABRS and AVRS can cause these symptoms, though sometimes higher temperatures are seen in bacterial infections. However, there's significant overlap. | |
Sinus tenderness on physical examination Hint: This is found in both ABRS and AVRS and lacks specificity. |
Question 2 |
Transillumination of sinuses Hint: Transillumination is used in the initial evaluation of chronic or acute sinusitis, but is not sensitive or specific. | |
Sinus X-ray Hint: Less sensitive than CT for soft tissue visualization (polyps, etc.) and doesn't provide the same detailed sinus anatomy view. | |
CT scan of sinuses | |
Nasal culture Hint: Nasal culture is not indicated in the evaluation of chronic sinus infections. | |
Allergy skin testing Hint: While allergies can predispose some to inflammation contributing to sinusitis, they aren't a primary initial assessment in suspected chronic sinusitis with this severity. |
Question 3 |
Streptococcus pneumoniae | |
Staphylococcus aureus Hint: While a potential cause of sinusitis, S. aureus is less common than S. pneumoniae in uncomplicated cases. It may be seen more frequently in chronic or complicated sinusitis. | |
Haemophilus influenzae Hint: H. influenzae is another significant cause of acute bacterial sinusitis, especially in children and those with underlying conditions. However, S. pneumoniae is still the most prevalent overall. | |
Pseudomonas aeruginosa Hint: P. aeruginosa is uncommon in community-acquired sinusitis. It's more frequently associated with hospital-acquired infections or immunocompromised patients. | |
Moraxella catarrhalis Hint: Similar to H. influenzae, M. catarrhalis contributes to acute bacterial sinusitis but is less common than S. pneumoniae as the primary agent. |
Question 4 |
Prescribe amoxicillin/clavulanate (Augmentin) | |
Prescribe azithromycin Hint: Both azithromycin and TMP-SMX are associated with high rates of bacterial resistance (because of overuse in patients with viral sinusitis ), and should only be used in patients who fail initial therapy or are allergic to penicillins. | |
Prescribe trimethoprim-sulfamethoxazole (TMP-SMX) Hint: Both azithromycin and TMP-SMX are associated with high rates of bacterial resistance (because of overuse in patients with viral sinusitis ), and should only be used in patients who fail initial therapy or are allergic to penicillins. | |
CT Head Hint: Imaging cannot differentiate viral from bacterial URI and generally does not change management in uncomplicated cases. It can be useful, though, in complicated cases or patients unresponsive to initial therapy. | |
Sinus aspiration Hint: Sinus aspiration is the gold standard for diagnosing a sinus infection as bacterial. However, it is invasive, time-consuming, painful for patients, and wholly unnecessary to diagnose and properly treat bacterial sinusitis. |
Question 5 |
Oral glucocorticoids Hint: While short courses of oral glucocorticoids may be considered for patients with persistent symptoms despite initial interventions, they are not recommended as the first-line treatment due to potential systemic side effects.
| |
Intranasal corticosteroids and high-volume saline irrigations | |
Extended course of macrolide antibiotics Hint: An extended course of macrolide antibiotics is considered for patients with persistent symptoms who have contraindications to surgery or recurrent symptoms following surgery, not as initial therapy. | |
Referral for functional endoscopic sinus surgery (FESS) Hint: FESS is suggested for patients with persistent symptoms despite nonsurgical interventions. It is not indicated as an initial treatment before attempting medical management. | |
Respiratory biologic therapy Hint: There are no approved biologic therapies for CRSsNP alone. Biologics may be considered in patients with coexistent conditions that can be treated with respiratory biologics, such as moderate-to-severe asthma, not as a first-line treatment for CRSsNP. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture


