NCCPA™ PANCE EENT Content Blueprint ⇒ ear disorders ⇒ inner ear
| Acoustic neuroma | Patient will present as → a 42-year-old male with a history of neurofibromatosis type II, complaining of nausea, vomiting, headache, continuous disequilibrium, and a slowly progressive unilateral hearing loss in his right ear. On physical exam, the patient has decreased sensation to touch on the right side of his face. An MRI is performed, with results seen here. Benign tumor of the Schwann cells (the cells which produce myelin sheath) – most commonly affects the vestibular division of the 8'th cranial nerve.
DX: Definitive diagnosis is by MRI (Gold standard)
TX: Surgery or stereotactic radiation therapy |
| Barotrauma | Patient will present as → a 17-year-old male who returned from a senior class trip to Mexico. While there, they decided to take scuba classes. After 3 days of shallow diving, they attempted their first 100-foot dive. After 5 minutes on their second dive, his equipment failed. He quickly shared the working breathing equipment of his friend, and they rose rapidly to the surface in a panic for air. The patient noticed immediate pain in his right ear, which resolved somewhat when he forcefully yawned and heard a “pop.” Since then, he reports dizziness and hearing loss in the affected ear. Barotrauma presents with ear pain and hearing loss that persists past the inciting event, associated with pressure changes
DX: clinical diagnosis but sometimes requires imaging tests
TX: Supportive (anti-inflammatories), then consider prophylaxis
|
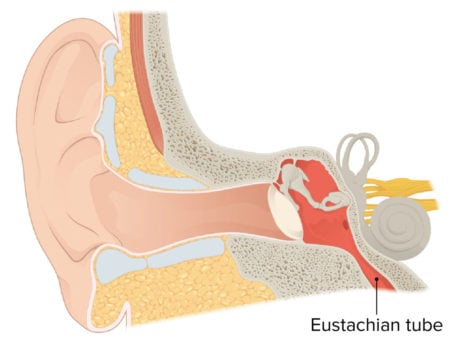
| Dysfunction of the eustachian tube | Patient will present as → a 9-year-old female with right otalgia and a nonproductive cough for one day. The patient complains of constant popping in her ears and fluctuating conductive hearing loss with tinnitus. The patient has no significant past medical history, her immunizations are up to date, and both of her parents are non-smokers. On otoscopic examination, the tympanic membranes are grey with normal landmarks, including visualization of the middle ear ossicles. There is no evidence of bulging pus or exudate suggestive of an acute inflammatory process. Ear fullness, popping of ears, underwater feeling, intermittent sharp ear pain, fluctuating conductive hearing loss, tinnitus.
DX: An excellent otoscopic exam is the key to making this diagnosis – otoscopic findings are usually normal. May see fluid behind TM if acute serous otitis media
TX: Often, no treatment is necessary |
| Labyrinthitis | Patient will present as → a 57 yo female with a six-day history of severe continuous dizziness associated with ataxia and right-sided hearing loss. She had an upper respiratory tract infection one week ago. Acute onset, continuous vertigo + hearing loss, tinnitus of several days to a week
DX: Labyrinthitis is a clinical diagnosis in the absence of neurologic deficits
TX:
Labyrinthitis is associated with CONTINUOUS vertigo along with hearing loss +/- tinnitus and is usually associated with an upper respiratory infection. This differentiates it from Meniere’s syndrome, which is EPISODIC and not typically associated with a viral infection. The features of acute labyrinthitis are similar to those of vestibular neuronitis, except labyrinthitis includes significant sensorineural hearing loss, which is NOT present in vestibular neuronitis. |
| Vertigo (ReelDx) | ReelDx Virtual Rounds (Vertigo )Patient will present as → a 29-year-old male with intense nausea and vomiting that began yesterday. He states that he ran a 5K race in the morning and felt well while resting afterward. However, when he arose, he experienced two episodes of emesis accompanied by a sensation that the world was spinning around him. This lasted about one minute and subsided. He denies tinnitus or hearing changes but feels imbalanced. He has a PMH of migraines, but he typically does not have nausea or vomiting with migraine episodes. His temperature is 98.7°F, blood pressure is 132/82 mmHg, pulse is 75/min, and respirations are 13/min. The cardiopulmonary exam is unremarkable. Cranial nerves are intact, and gross motor function and sensation are within normal limits. When the patient’s head is turned to the right side and lowered quickly to the supine position, he claims that he feels “dizzy and nauseous.” Nystagmus is noted in both eyes. The sensation of movement (spinning, tumbling, or falling) in the absence of actual movement or an overresponse to movement
Central vertigo
Peripheral vertigo (inner ear)
DX:
Treatment:
|
Clinical features of peripheral versus central vertigo
| Peripheral | Central | |
| Nystagmus | ||
| Features (direction and type) | Unidirectional, fast component toward the normal ear; never reverses direction
Horizontal with a torsional component; never purely torsional or vertical |
Sometimes reverses direction when patient looks in the direction of slow component
Can be any direction; note that purely vertical or purely torsional nystagmus is a central sign |
| Effect of visual fixation | Suppressed | Not suppressed |
| Postural instability | Unidirectional instability, walking preserved | Severe instability, patient often falls when walking |
| Deafness or tinnitus | May be present | Usually absent |
| Other neurologic signs and symptoms | Absent | Often present (eg, diplopia, ataxia, dysarthria, dysphagia, focal or lateralized weakness) |
| Disease | Characteristics | Symptoms | Diagnostic Test | Treatment |
| Benign positional vertigo | Changes with position | Vertigo without hearing loss, tinnitus, or ataxia | MRI of the internal auditory canal | Diagnosis: Dix-Hallpike maneuver
Treatment: Epley maneuver Meclizine |
| Vestibular neuritis | Vertigo without position changes | Vertigo but no hearing loss or tinnitus (inflammation of vestibular portion of CN VIII) associated with URI | Meclizine | |
| Labyrinthitis | Acute, self-resolving episode | Continuous Vertigo
Hearing loss Tinnitus Self-limited Associated with URI |
Meclizine + steroids | |
| Meniere's disease | Chronic remitting and relapsing episodes | Episodic Vertigo
Hearing loss Tinnitus and chronic remitting and relapsing manner Not associated with URI |
Diuretics
Salt restriction Unilateral CN VIII ablation (severe cases) |
|
| Acoustic neuroma | Ataxia
Neurofibromatosis type II MRI findings Facial numbness |
Vertigo
Unilateral hearing loss Tinnitus AND ataxia |
Surgical intervention |