Patient with dacryoadenitis will present as → a 32-year-old woman presents to the emergency department with a 2-day history of pain, redness, and swelling in the outer corner of her right eye. She denies any vision changes, discharge, or trauma. She has no significant past medical history and is not on any medications. On physical examination, you note localized erythema and swelling over the lateral aspect of her right upper eyelid. Her visual acuity is normal, and there is no proptosis.
Patient with dacryocystitis will present as → a 58-year-old woman presents to the emergency department with a 3-day history of increasing pain, redness, and swelling in the inner corner of her left eye. She also reports some purulent discharge from the same eye. She denies any vision changes or trauma. On physical examination, you note localized erythema, warmth, and swelling over the medial canthal area of her left eye. Her visual acuity is normal.
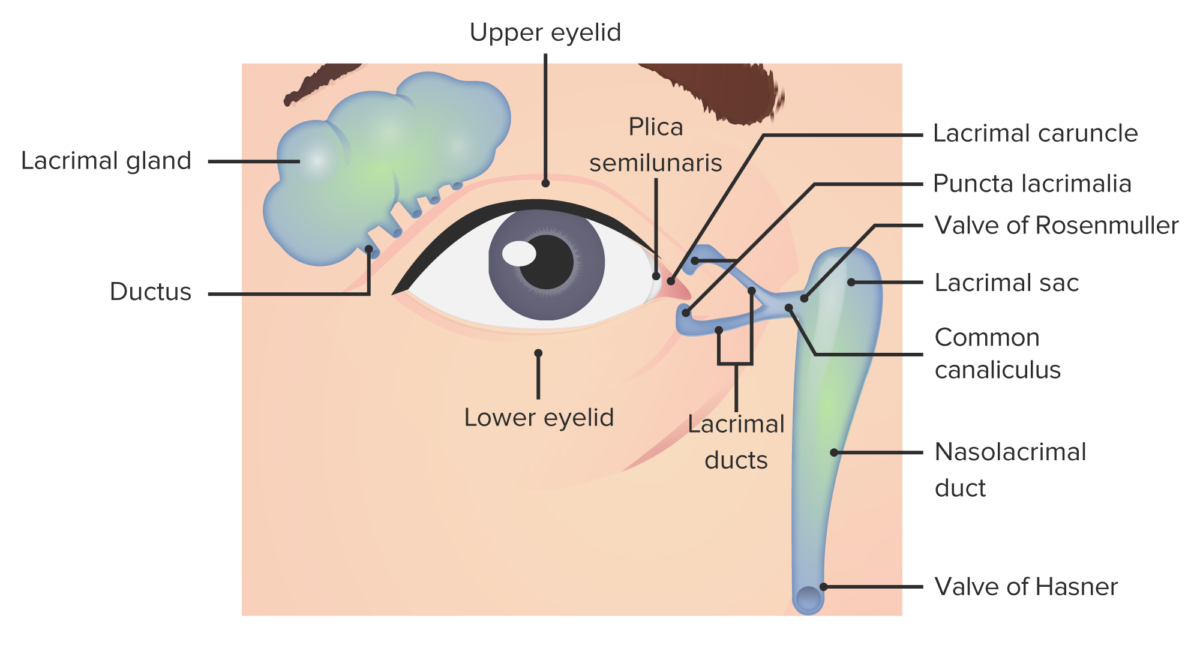
Dacryoadenitis is inflammation of lacrimal (tear-producing) glands usually caused by bacteria or a virus that initiates the inflammation (supratemporal)
- s/sx: unilateral severe pain, swelling, redness, tearing, drainage
- Acute dacryoadenitis is most commonly due to viral or bacterial infection. Common causes include mumps, Epstein-Barr virus, staphylococcus, and gonococcus.
- Chronic dacryoadenitis is most often due to noninfectious inflammatory disorders. Examples include sarcoidosis, thyroid eye disease, and orbital pseudotumor.
"On the boards you may be able to differentiate between the two based on the location: dacryocystitis will be medial. Remember, medial = Center = dacroCystitis. vs. dacryoAdenitis, which is up, up, and Away. Also, it's important to note that dacryocystitis affects the duct, and dacryoadenitis affects the gland."
Dacryocystitis is an infectious obstruction of the nasolacrimal duct (inferomedial region)
- Dacryocystitis will be medial (remember "c" for central)
- There will be an overflow of tears because the nasolacrimal duct is obstructed, and there is nowhere for the fluid to exit
- Often caused by a stone, debris, or dacryostenosis (would be seen in small children) = congenital malformation or failure of duct to open
- Dacryoadenitis may lead to dacryocystitis and periorbital cellulitis if untreated – redness to the nasal side of the lower lid
The diagnosis of dacryocystitis and dacryoadenitis based on clinical observation
- In cases of chronic dacryoadenitis/dacryocystitis, a CT or MRI of the orbits may be warranted
- In acute cases of dacryocystitis, a tear duct massage can be performed to express material for culture and gram stain
- In patients who appear to be acutely toxic or those who present with visual changes, imaging, and bloodwork should be considered
Dacryoadenitis
- If the cause of dacryoadenitis is a viral condition such as mumps, simple rest and warm compresses may be all that is needed
- For other causes, the treatment is specific to the causative disease
Dacryocystitis
- Acute dacryocystitis (< 3 months) is treated with systemic antibiotics
- Chronic dacryocystitis (> 3 months) typically presents with fewer inflammatory signs and requires surgical therapy for the underlying cause
Question 1 |
A 7-month-old female is brought to your clinic by her mother, who is concerned about persistent swelling at the nasal corner of the child's left eye. The mother reports that the swelling has been present for several weeks and occasionally becomes red and inflamed. If this condition is left untreated, which of the following complications is most likely to develop?
Hyphema Hint: This refers to the presence of blood in the anterior chamber of the eye, typically resulting from trauma or eye surgery, not related to nasolacrimal duct obstruction. | |
Papilledema Hint: This is swelling of the optic disc due to increased intracranial pressure and is not a complication associated with nasolacrimal duct obstruction. | |
Pterygium Hint: A pterygium is a benign growth on the conjunctiva that can encroach onto the cornea, usually related to UV light exposure, not nasolacrimal duct issues. | |
Dacryocystitis | |
Orbital Cellulitis Hint: While severe untreated eye infections can potentially lead to orbital cellulitis, it is less likely in this scenario without evidence of a more significant or spreading infection. |
Question 2 |
Location of swelling: Dacryoadenitis - lateral canthus, Dacryocystitis - medial canthus. | |
Discharge: Dacryoadenitis - mucopurulent, Dacryocystitis - purulent. Hint: While both can have purulent discharge, it's not a reliable differentiator. | |
Tenderness: Dacryoadenitis - absent, Dacryocystitis - present upon lacrimal sac palpation. Hint: Both conditions can have tenderness, though lacrimal sac palpation in Dacryocystitis might be more pronounced. | |
Fever: Dacryoadenitis - common, Dacryocystitis - rare. Hint: Fever can be present in both, especially with infections. | |
Lacrimation: Dacryoadenitis - decreased, Dacryocystitis - increased. Hint: Dacryoadenitis typically presents with decreased tear production, while Dacryocystitis can have either increased or decreased tears depending on the cause and obstruction. |
Question 3 |
Intravenous antibiotics | |
Warm compresses and continued oral antibiotics Hint: Appropriate for mild cases but not for worsening symptoms. | |
Dacryocystorhinostomy Hint: A surgical procedure indicated for chronic dacryocystitis or obstruction, not acute infection. | |
Topical corticosteroids Hint: Not indicated in acute infections and can potentially worsen the condition. | |
Incision and drainage of the lacrimal sac Hint: Typically reserved for abscess formation or severe cases not responding to intravenous antibiotics. |
Question 4 |
Intravenous antibiotics | |
Warm compresses and continued oral antibiotics Hint: Appropriate for mild cases but not for worsening symptoms. | |
Dacryocystorhinostomy Hint: A surgical procedure indicated for chronic dacryocystitis or obstruction, not acute infection. | |
Topical corticosteroids Hint: Not indicated in acute infections and can potentially worsen the condition. | |
Incision and drainage of the lacrimal sac Hint: Typically reserved for abscess formation or severe cases not responding to intravenous antibiotics. |
|
List |
References: Merck Manual · UpToDate