NCCPA™ PANCE EENT Content Blueprint ⇒ Disorders of the eye
 Osmosis Osmosis |
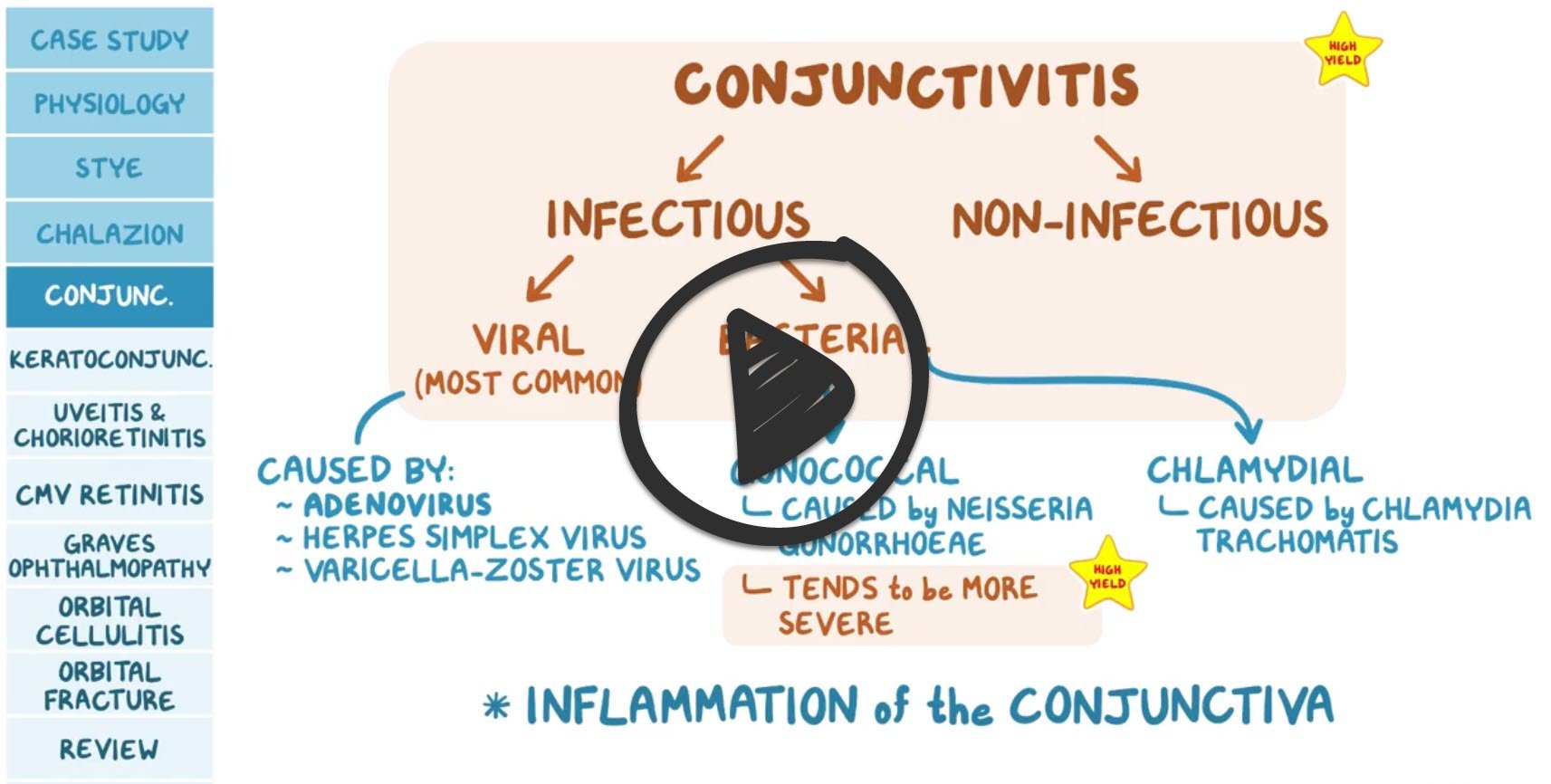 |
| Conjunctivitis | ReelDx Virtual Rounds (Conjunctivitis )Patient will present as → a 6-year-old boy complaining of itchy eyes. The mother states that she has noted that he has been tearing and that both of his eyes have been red for the past 4 days. The patient denies any pain but has had a runny nose for the past week. The mother states that he has not had any sick contacts, and he has been home from school for summer vacation. On exam, there is marked redness, tearing, and eyelid edema of both eyes. Viral conjunctivitis - copious watery discharge, scant mucoid discharge. Adenovirus (most common). Self-limiting associated with URI Bacterial conjunctivitis - will present with purulent (yellow) discharge, crusting, usually worse in the morning. It may be unilateral.
Allergic conjunctivitis - red eyes, itching and tearing, usually bilateral, cobblestone mucosa on the inner/upper eyelid TX: Bacterial: Treatment(s) in order of suggested use - the dose is 0.5 inch (1.25 cm) of ointment (preferable in children) deposited inside the lower lid or 1 to 2 drops instilled four times daily for five to seven days.
Contact lenses use = pseudomonas tx=fluoroquinolone (ciprofloxacin / Ciloxan drops)
Viral: There is no specific antiviral agent for the treatment of viral conjunctivitis. Some patients derive symptomatic relief from topical antihistamine/decongestants. Warm or cool compresses may provide additional symptomatic relief. Allergic conjunctivitis systemic antihistamines and topical antihistamines or mast cell stabilizers. (Naphcon-A, Ocuhist, generics)
|
| Cataract | Patient presents as → a 78-year-old man who complains of slowly progressive vision loss over the last several years. He describes his vision as if he is looking through “dirty glass” and reports seeing a white halo around lights. On physical exam, there is clouding of the lens and no red reflex. Blurred vision over months or years, halos around lights. Clouding of the Lens (versus clouding of cornea = glaucoma)
DX: is by fundoscopy "black on red background" ⇒ cataract appears dark against the red reflex on exam
Tx: Surgical removal is definitive |
| Corneal ulcer | Patient will present as → a 34-year-old contact lens wearer with severe pain, redness, and photophobia. Eyes are injected with cloudy discharge unilaterally. A dense corneal infiltrate is visible with fluorescein staining. Contact lens wearers - caused by a deep infection in the cornea by bacteria, viruses, or fungi.
DX: Fluorescein stain is diagnostic
TX: Immediate referral - if an immediate referral is not possible, it is reasonable to start topical ophthalmic antibiotics without delay Corneal Ulcers vs. Keratitis The main difference between a corneal ulcer and keratitis is that a corneal ulcer is an open sore on the cornea, while keratitis is a general term for inflammation of the cornea. Not all cases of keratitis lead to corneal ulcers, but a corneal ulcer is always accompanied by keratitis!
|
| Keratitis | Patient will present as → a 37-year-old female with intense, tearing pain in her right eye. She was recently placed on topical corticosteroids for suspected allergic conjunctivitis. On visual inspection, the conjunctiva appears red. A fluorescein stain of the eye exhibits a shallow ulcer with a dendritic appearance and irregular borders. Keratitis is a condition in which the cornea becomes inflamed and is often marked by pain, impaired eyesight, photophobia, and red eye
DX: With fluorescein staining of the cornea, epithelial herpes keratitis is characterized by the presence of dendritic lesions
TX: Treat herpes keratitis with topical antiviral
|
| Pterygium | ReelDx Virtual Rounds (Pterygium)Patient will present as → a 65-year-old male Hispanic farmworker who is brought to you by his concerned wife. She reports he has had this “thing” on his left eye for years and refuses to seek care. He denies pain or discharge from the affected eye. Physical exam reveals an elevated, superficial, fleshy, triangular-shaped fibrovascular mass in the inner corner/nasal side of the left eye. Elevated, superficial, fleshy, triangular-shaped “growing” fibrovascular mass (most common in the inner corner/nasal side of the eye).
DX: This is a clinical diagnosis TX: Only surgically remove when vision is affected |
| Dacryoadenitis and Dacryocystitis | Patient will present as → a 12-year-old with severe unilateral right eye pain and pressure. On physical exam, there is swelling, redness, tearing, and drainage from the outermost part of the affected right eye.
TX:
Dacryocystitis
DX:
TX:
|
| Blepharitis | Patient will present as → a 34-year-old female with crusting, scaling, red-rimming of the eyelid, and eyelash flaking along with dry eyes. The patient has a history of seborrhea and rosacea. Eyelid changes: crusting, scaling, red-rimming of the eyelid, and eyelash flaking along with dry eyes and associated seborrhea and rosacea DX: Diagnosis is usually by slit-lamp examination
TX: Warm compresses, irrigation, lid massage, and topical antibiotics for flare-ups
|
| Chalazion | Patient will present as → a 52-year-old male with a foreign-body sensation in the right eye. Over the last 3 weeks, he has had gradually increasing painless swelling around the right lower eyelid. Your examination shows a nontender discrete nodule on the right lower eyelid. There is no evidence of injection or discharge, and her visual acuity is normal. A chalazion is a sterile, painless (non-infectious) granuloma of the internal meibomian sebaceous gland, a painless "cold" lid nodule DX: Diagnosis is clinical
TX: Warm compresses and eyelid hygiene
|
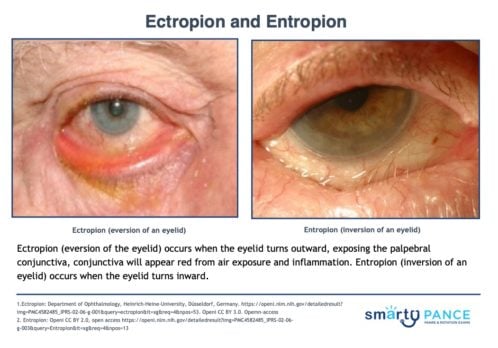
| Ectropion | Patient will present as → a 72-year-old with complaints of dry eyes coupled with excessive tearing. On exam, the conjunctiva appears red, and the left eyelid is turned outward. Ectropion (eversion of the eyelid) occurs when the eyelid turns outward, exposing the palpebral conjunctiva. The conjunctiva will appear red from air exposure and inflammation. DX: Diagnosis is clinical (the eyelid turns out) TX: Tear supplements and ocular lubricants at night
|
| Entropion | Patient will present as → a 75-year-old with a foreign body sensation and tearing of his right eye. On physical exam, you note a red, irritated right eye in association with an inverted eyelid. Entropion (inversion of an eyelid) occurs when the eyelid turns inward. It is most commonly caused by age-related tissue relaxation, surgical correction is definitive DX: Diagnosis is clinical (eyelids turn in) TX: Tear supplements and ocular lubricants at night
|
| Hordeolum | ReelDx Virtual Rounds (Hordeolum )Patient will present as → a 15-year-old male with pain, redness, and swelling of the upper eyelid for the last 3 days. There are no visual changes or photophobia. Examination reveals a tender, erythematous, and outward-pointing edema of the right eyelid. Painful, warm (hot), swollen red lump on the eyelid (different from a chalazion, which is painless)
DX: The diagnosis is clinical TX: Warm compress and topical antibiotics
|
| Nystagmus | ReelDx Virtual Rounds (Nystagmus)Patient will present as → a 46-year-old male with an involuntary, rapid, and repetitive movement of both eyes side to side. Involuntary, jerking movements of the eyes
DX: Caloric reflex test in which one ear canal is irrigated with warm or cold water or air. The temperature gradient provokes the stimulation of the horizontal semicircular canal and the consequent nystagmus.
TX: medications baclofen and gabapentin
|
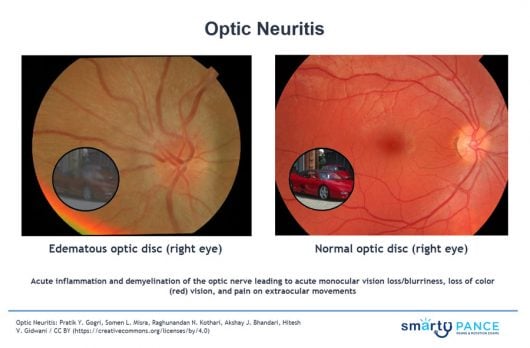
| Optic neuritis (ReelDx) | ReelDx Virtual Rounds (Optic neuritis )Patient will present as → a 47-year-old school teacher with a cough, hemoptysis, fever, chills, and weight loss that has persisted since he returned from a summer trip to China. A chest radiograph is concerning for infection, and a sputum culture is positive for acid-fast organisms. Treatment for this patient’s condition is begun. Three weeks later, the patient returns to the clinic with decreased visual acuity for one day in his right eye. He also reports pain in the eye with movement but no other symptoms. The patient has a family history of glaucoma, diabetes mellitus, factor V Leiden, and stroke. On physical examination, when a penlight is shined into the affected eye, there is no pupillary constriction in either eye. Acute inflammation and demyelination of the optic nerve leading to acute monocular vision loss/blurriness and pain on extraocular movements
DX: Fundoscopy ⇒ inflammation of the optic disc
TX: IV corticosteroids
|
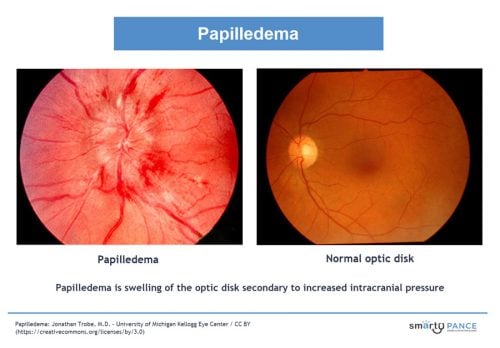
| Papilledema (ReelDx) | ReelDx Virtual Rounds (Papilledema)Patient will present as → a 57-year-old male with a history of hypertension who complains of an acute onset of intermittent headaches and blurred vision of the right eye. Optic disc swelling that is caused by increased intracranial pressure. The swelling is usually bilateral and can occur over a period of hours to weeks
DX: Diagnosis is by ophthalmoscopy with further tests, usually brain imaging and sometimes subsequent lumbar puncture, to determine the cause
TX: Treat underlying cause |
| Orbital cellulitis (ReelDx) | ReelDx Virtual Rounds (Orbital cellulitis)Patient will present as → a 2-year-old who arrives at the ED with a swollen and erythematous eyelid, proptosis, pain with movement of the eye, and an inability to adduct or abduct his eye. Orbital cellulitis is a serious infection of the eye and the eye structures within the bony cavity of the face. Symptoms include swelling, redness, and pain around the eye, as well as decreased eye movement and vision.
DX: history, clinical exam, and focused assessment of extraocular muscles
TX: Hospitalization and IV broad-spectrum antibiotics |
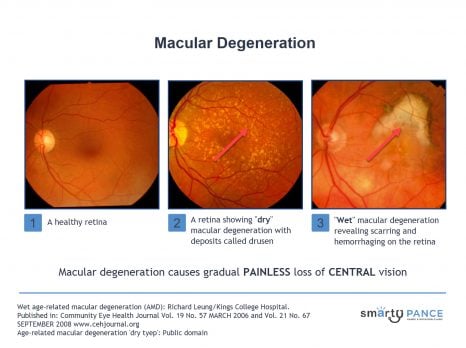
| Macular degeneration | Patient will present as → a 62-year-old male who arrives for his follow-up visit for chronic central visual loss. He describes a phenomenon of wavy or distorted vision that has deteriorated rather quickly. The patient is frustrated because he “just can’t drive anymore,” and he is “having difficulty seeing words when he reads.” When looking at a specific region of the Amsler grid, he reports a dark “spot” in the center, with bent lines. On the fundoscopic exam, you note areas of retinal depigmentation along with the presence of yellow retinal deposits. Gradual painless loss of central vision. The macula is responsible for central visual acuity, which is why macular degeneration causes gradual central field loss.
DX: funduscopic findings are diagnostic; color photographs, fluorescein angiography, and optical coherence tomography assist in confirming the diagnosis and in directing treatment. TX: Wet age-related macular degeneration
Dry age-related macular degeneration
|
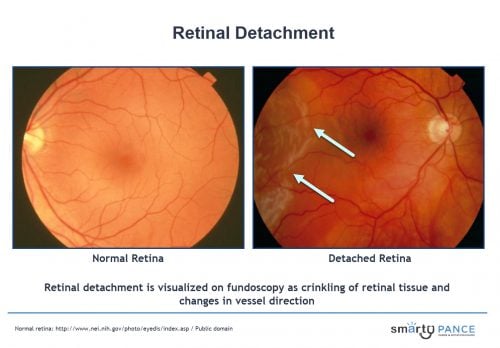
| Retinal detachment | Patient will present as → a 65-year-old man complaining of a sudden unilateral vision loss, which he describes as a “curtain or dark cloud lowering over my eye.” This was preceded by small moving flashing lights and floaters. The fundoscopic exam reveals a detached superior retina. Separation of the retina from the pigmented epithelial layer causing the detached tissue to appear as a flap in the vitreous humor
DX: is by fundoscopy
TX: Retinal detachment is an ophthalmologic emergency
|
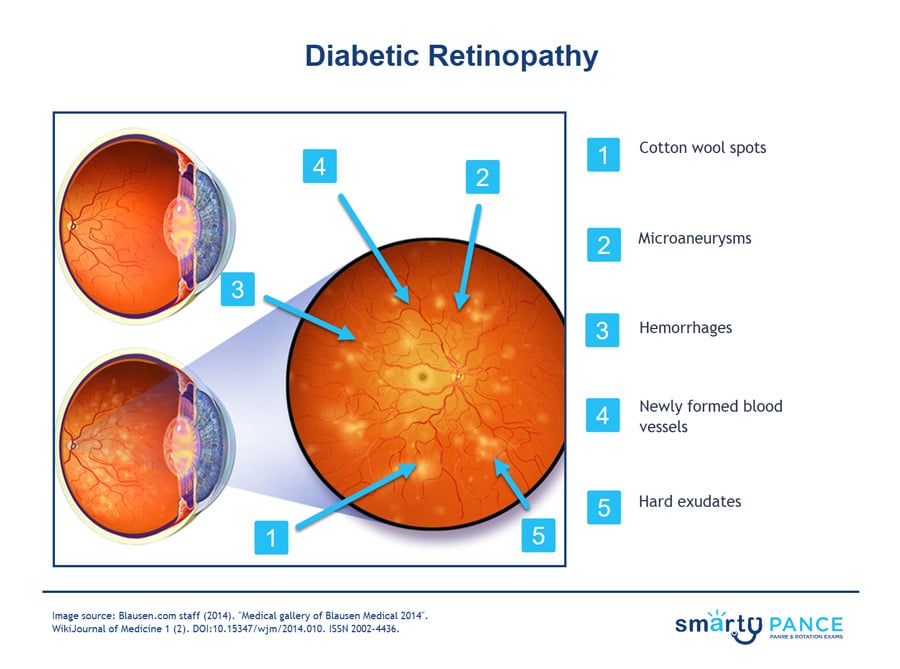
| Retinopathy | Patient will present as → a 65-year-old woman with a 10-year history of type 2 diabetes mellitus presents for a routine eye examination. She reports no visual symptoms. Her last eye examination was 2 years ago. On fundoscopic examination, you note microaneurysms, dot and blot hemorrhages, and hard exudates in both eyes. There is no evidence of neovascularization or vitreous hemorrhage. Caused by systemic disorders, including diabetes, hypertension, preeclampsia-eclampsia, blood dyscrasias, and HIV disease -may affect the retina
Hypertensive retinopathy is retinal damage caused by high blood pressure.
Nonproliferative type (an early form of the disease)
Proliferative type (most severe, abnormal blood vessel growth)
TX: control of blood glucose and BP
|
| Blowout fracture (ReelDx) | ReelDx Virtual Rounds (Blowout fracture)Patient will present as → a 13-year-old who was hit in the right eye by a baseball. The area is ecchymotic and swollen. He complains of pain, rated 6 out of 10. On physical exam, the patient has eyelid swelling, decreased visual acuity, enophthalmos (sunken eye), and anesthesia/paresthesia in the gums and upper lips. History of blunt trauma, muscle entrapment, eyelid swelling, gaze restriction, double vision, decreased visual acuity, enophthalmos (sunken eye)
DX: diagnosed with CT scan TX: Prompt ophthalmic referral ⇒ treatment with surgery
|
| Corneal abrasion (ReelDx) | ReelDx Virtual Rounds (Corneal abrasion)Patient will present as → a 10-year-old boy who was hit in the right eye with a piece of bark that was thrown on the playground. He developed a sudden onset of eye pain, photophobia, tearing, and blurring of vision. He claims there is “something stuck in my eye.” On physical examination, there is significant conjunctival injection. Sudden onset of eye pain, photophobia, tearing, foreign body sensation, blurring of vision, and/or conjunctival injection DX: fluorescein staining - increased absorption in the devoid area TX: Antibiotic eye ointment, no patching |
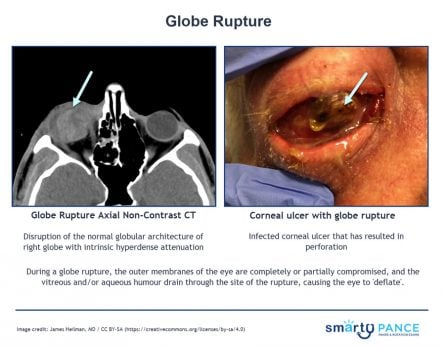
| Globe Rupture | Patient will present as → a 15-year-old male with no significant PMHx is brought to the emergency department by his coach after being struck in the right eye by a baseball. The patient reports pain in the right eye with complete loss of vision. On physical examination, you note scleral buckling, and the visual acuity testing reveals light perception only. Globe rupture occurs when the integrity of the outer membranes of the eye is disrupted by blunt or penetrating trauma
DX: CT scan: non-contrast 1 to 2 mm cuts axial and coronal through the orbits TX: Avoid any examination procedure that might apply pressure to the eyeball, such as eyelid retraction or intraocular pressure measurement by tonometry
|
| Hyphema (ReelDx) | ReelDx Virtual Rounds (Hyphema )Patient will present as → a 14-year-old who sustained blunt trauma to his right eye after being struck by a baseball. He complains of blurry vision. On physical exam, you note unequal pupils, injected conjunctiva/sclera, and blood in the anterior chamber of the right eye. Trauma causes blood in the anterior chamber of the eye (between the cornea and the iris) and may cover the iris
DX: orbital CT if indicated + ophthalmology consult TX: usually, blood is reabsorbed over days/weeks
|
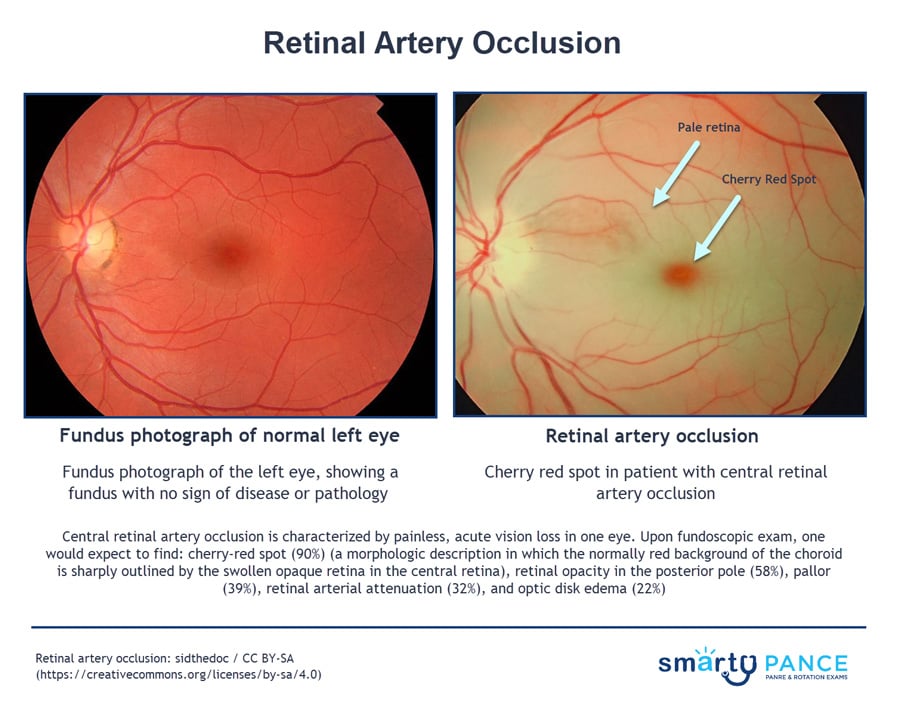
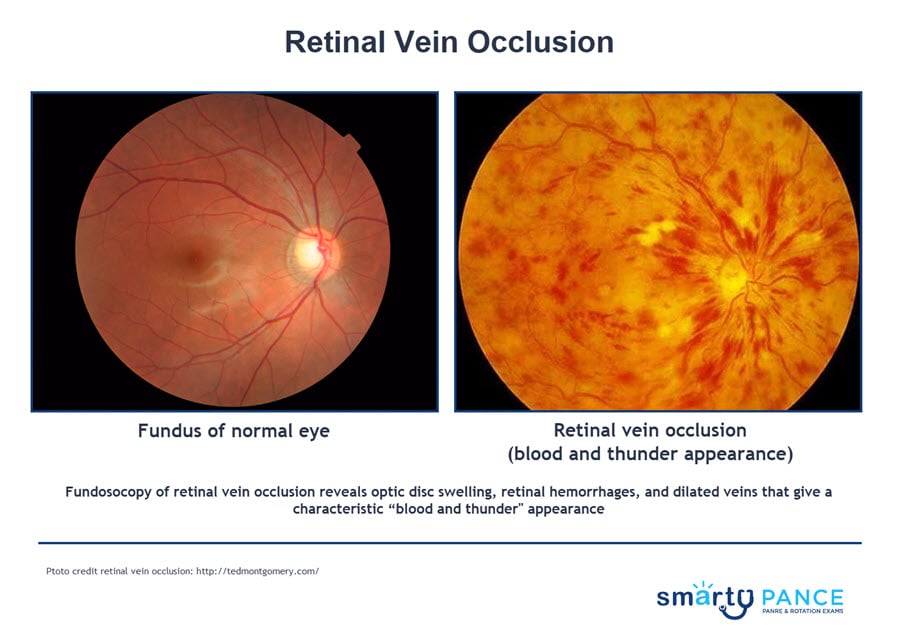
| Retinal vascular occlusion | Patient will present as → a 74-year-old man with sudden vision loss in his right eye. He has a medical history of hypertension, coronary artery disease, and new-onset atrial fibrillation. On physical exam, a carotid bruit is auscultated. His visual acuity is light perception. Confrontational visual fields reveal a dense scotoma, and a penlight examination shows an afferent pupillary defect. Dilated funduscopic examination shows retinal whitening with a cherry-red spot in the fovea. Central retinal artery occlusion (cherry-red spot, ischemic retina)
DX: Fundoscopy
TX: Emergent ophthalmologic consult - Immediate treatment is indicated if occlusion occurs within 24 hours of presentation
Central retinal vein occlusion (blood and thunder fundus)
DX: Funduscopy: retinal hemorrhages in all quadrants, optic disc swelling; blood and thunder retina (dilated veins, hemorrhages, edema, exudates) TX: vision resolves with time (partially); workup for thrombosis
|
| Amaurosis fugax | Patient will present as → an 82-year-old man who presents to the emergency department complaining of vision loss in his left eye. He states that it suddenly appeared as if a curtain was coming down over his left eye. It resolved after five minutes, and his vision has returned to normal. He has a history of coronary artery disease and type 2 diabetes. Amaurosis fugax (amaurosis meaning darkening, dark, or obscure, fugax meaning fleeting) is a painless temporary loss of vision in one or both eyes
Five distinct classes based on their supposed cause: embolic, hemodynamic, ocular, neurologic, and idiopathic
DX: A fundus exam may reveal optic disk pallor, a cherry-red macula (retinal vascular occlusion), and retinal edema
TX: If the diagnostic workup reveals a systemic disease process, directed therapies to treat that underlying cause should be initiated
|
| Amblyopia | Patient will present as → a 5-year-old male is brought by his parents and referred by his teacher for suspected decreased vision in his left eye. His mother had not noticed any vision problems. He has had normal growth and development. On exam, the patient has an abnormal vision screen of the left eye and red reflex asymmetry. Amblyopia (lazy eye) is reduced visual acuity that is not correctable by refractive means
DX: screening to detect amblyopia in all children younger than five years of age
TX: Includes correction of refraction error as well as forced use of the amblyopic eye by patching the better eye or blurring with glasses or drops |
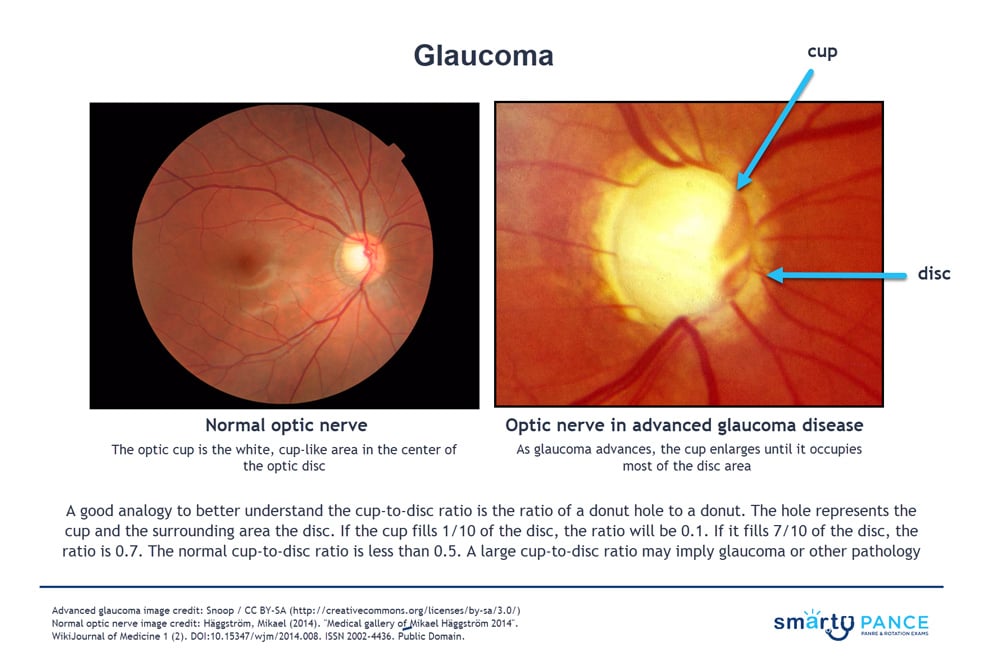
| Glaucoma | Patient with open-angle glaucoma present as → a 47-year-old African American male presents for an ophthalmic examination. Medical history is significant for hypertension and type II diabetes mellitus. On slit-lamp examination, there is cupping of the optic disc, with a cup-to-disc ratio > 0.6. Tonometry reveals intraocular pressure of 45 mmHg (normal is 8-21 mmHg). Peripheral field vision loss is noted on the visual field exam. Patient with acute angle-closure glaucoma will present with → a 60-year-old Asian American woman presents with sudden ocular pain. She reports she was visiting the planetarium when the pain started, and when she walked outside, she saw halos around the street lights. The pain was so bad that she began to vomit. She reports her vision is decreased. Physical examination reveals conjunctival injection, a cloudy cornea, and pupils Open-angle glaucoma: most common, aqueous outflow obstruction
Acute narrow angle-closure glaucoma: Iris against the lens, dark environment, acute loss of vision, nausea, and vomiting.
DX: Diagnosis is confirmed by tonometry demonstrating increased intraocular pressure
All patients should be screened at age 40 - may present for routine fundoscopy with a cup-to-disk ratio > 0.5 (<0.5 is normal). This is suggestive but not diagnostic of glaucoma, so you will progress to the next step, which is tonometry
TX: Acute narrow angle-closure glaucoma
Chronic open-angle glaucoma
|
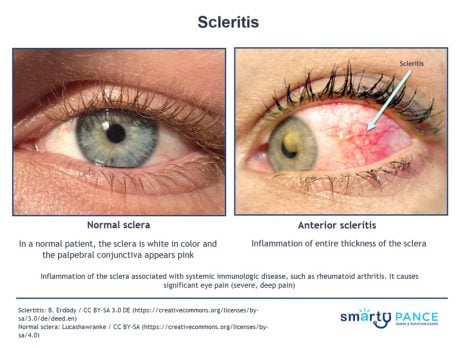
| Scleritis | Patient will present as → a 42-year-old white female complaining of a severely painful right eye. The pain is a constant, boring pain that worsens at night and in the early morning hours and radiates to the face and periorbital region. Additionally, she reports a headache, watering of the eye, and ocular redness. Inflammation of the sclera associated with systemic immunologic disease, such as rheumatoid arthritis
DX: On examination, there is ocular redness and pain on palpation of the eyeball. It can cause visual impairment
TX: Refer the patient for prompt evaluation by an ophthalmologist
|
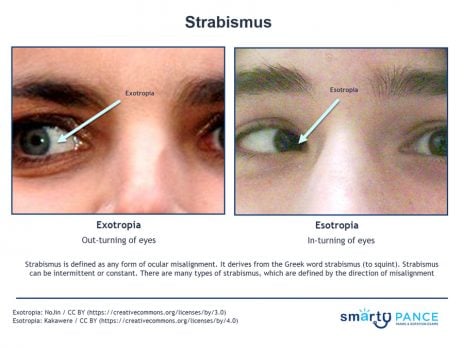
| Strabismus (ReelDx) | ReelDx Virtual Rounds (Strabismus )Patient will present as → a 3-year-old girl brought to you by her mother, who is worried about her daughter’s “lazy eye.” She reports that her daughter’s symptoms are exaggerated when she has a cold. Past medical history is negative for trauma or headaches. The patient has an asymmetric corneal light reflex, and the cover/uncover test reveals a right-sided esotropia. You refer the patient to a pediatric ophthalmologist. Strabismus is defined as any form of ocular misalignment
DX: The cover/uncover test is used to diagnose strabismus TX: Treatment options can include glasses, occlusion therapy, orthoptic exercises, surgery, or a combination of these therapies |