Patient will present as → a 5-year-old male is brought by his parents and referred by his teacher for suspected decreased vision in his left eye. His mother had not noticed any vision problems. He has had normal growth and development. On exam, the patient has an abnormal vision screen of the left eye and red reflex asymmetry.
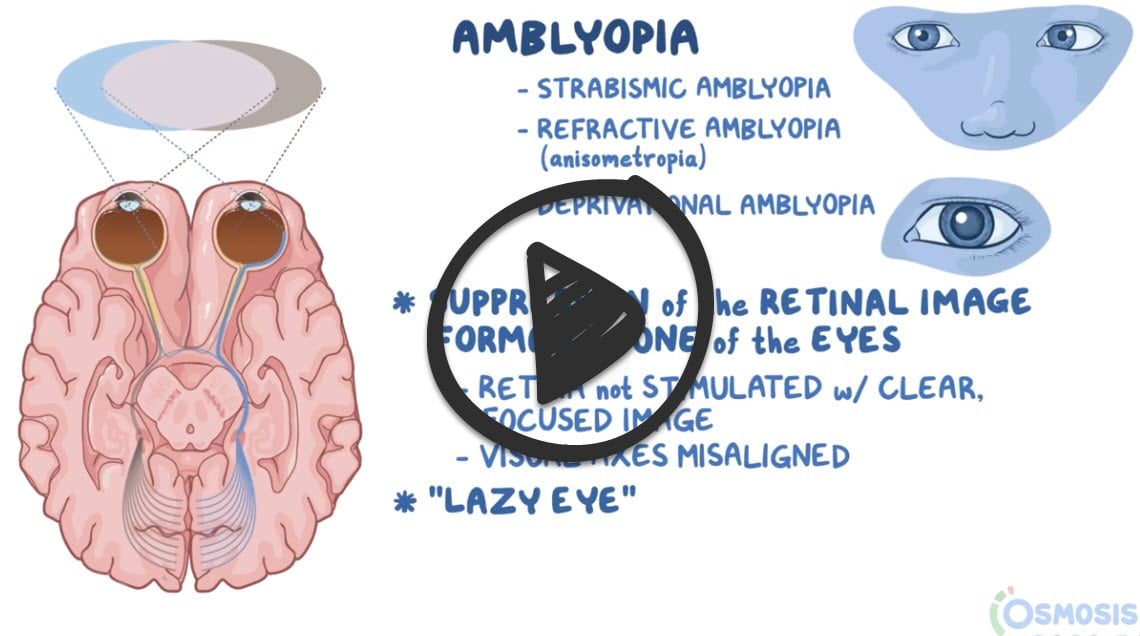
Amblyopia, also called lazy eye, is a disorder of sight in which the brain fails to process inputs from one eye and over time favors the other eye. It results in decreased vision in an eye that otherwise typically appears normal
- Amblyopia is not correctable by refractive means
- Amblyopia occurs in early childhood when nerve pathways between the brain and an eye aren't properly stimulated ⇒ the brain favors the other eye
- It may be caused by strabismus (crossed eye); uremia; or toxins, such as alcohol, tobacco, lead, and other toxic substances
- Symptoms include a wandering eye, eyes that may not appear to work together, poor depth perception, blurred vision, or double vision. Both eyes may be affected
Screening to detect amblyopia should be performed in all children younger than five years of age
- Screening includes vision risk assessment at all health maintenance visits and vision screening at age three, four, and five
- Diagnosis of amblyopia requires visual acuity testing, which should result in 20/40 vision in either eye in children > 4 years or worse than 20/50 those in < 3 years
- Tests to detect the cause of amblyopia include the red reflex test; stereopsis testing; the Titmus test; assessment of ocular fixation, alignment, and motility for strabismus; a slit lamp exam to detect deprivational amblyopia; and cycloplegic and dilated fundoscopy to detect other pathologies
Treatment includes correction of refraction error as well as forced use of the amblyopic eye by patching the better eye
- Some children cannot tolerate the patch, in which case the good eye is blurred with glasses or drops (penalization therapy) to stimulate proper visual development of the more severely affected eye
- It is more resistant to treatment at an older age; thus, children should be treated early
Question 1 |
Congenital cataracts noted at birth Hint: Congenital cataracts can occur in newborn babies for many reasons, including inherited tendencies, infection, metabolic problems, diabetes, trauma, inflammation or drug reactions. As an example, tetracycline antibiotics used to treat infections in pregnant women have been shown to cause cataracts in newborn babies. | |
Retinal detachment seen in premature children Hint: When a baby is born prematurely, the retinal blood vessels can grow abnormally. Most Retinopathy of prematurity (ROP) resolves without causing damage to the retina. When ROP is severe, it can cause the retina to pull away or detach from the wall of the eye and possibly cause blindness. | |
Irregular pupillary size Hint: Unequal pupil size is called anisocoria. If pupil sizes are very unequal, a person may notice the discrepancy. More often, unequal pupils are noticed only during an examination. Unequal pupils themselves usually cause no symptoms, but occasionally a person may have trouble focusing on near objects. | |
Increased distance between the medial and lateral canthus Hint: Telecanthus, or dystopia canthorum, refers to increased distance between the inner corners of the eyelids (medial canthi), while the inter-pupillary distance is normal. Telecanthus is often associated with many congenital disorders. Congenital disorders such as Down syndrome, fetal alcohol syndrome, cri du chat syndrome, Klinefelter syndrome, Turner syndrome, Ehlers–Danlos syndrome, Waardenburg syndrome often present with prominent epicanthal folds, and if these folds are nasal (as they most commonly are) they will cause telecanthus | |
Subnormal visual acuity in one or both eyes despite correction of refractive error |
Question 2 |
Immediate surgical correction of the esotropia Hint: Not indicated as initial treatment at this age. | |
Start part-time occlusion therapy of the right eye | |
Prescribe corrective lenses and yearly follow up Hint: Occlusion therapy is essential and should begin right away. | |
Observation without treatment at this time Hint: Risks permanent vision impairment in the amblyopic eye. | |
Begin vision therapy and occupational therapy Hint: Occlusion therapy is the initial treatment of choice. |
|
List |
References: Merck Manual · UpToDate