
A 6-year-old girl with increasing bilateral nosebleeds over the past week
Patient will present as → a 13-year-old boy with clear fluid discharge from his nose for 2 days duration. This has also been associated with sneezing. On nasal exam, the mucosa and turbinates appear edematous and slightly bluish. He has swollen dark circles under his eyes and a transverse nasal crease.
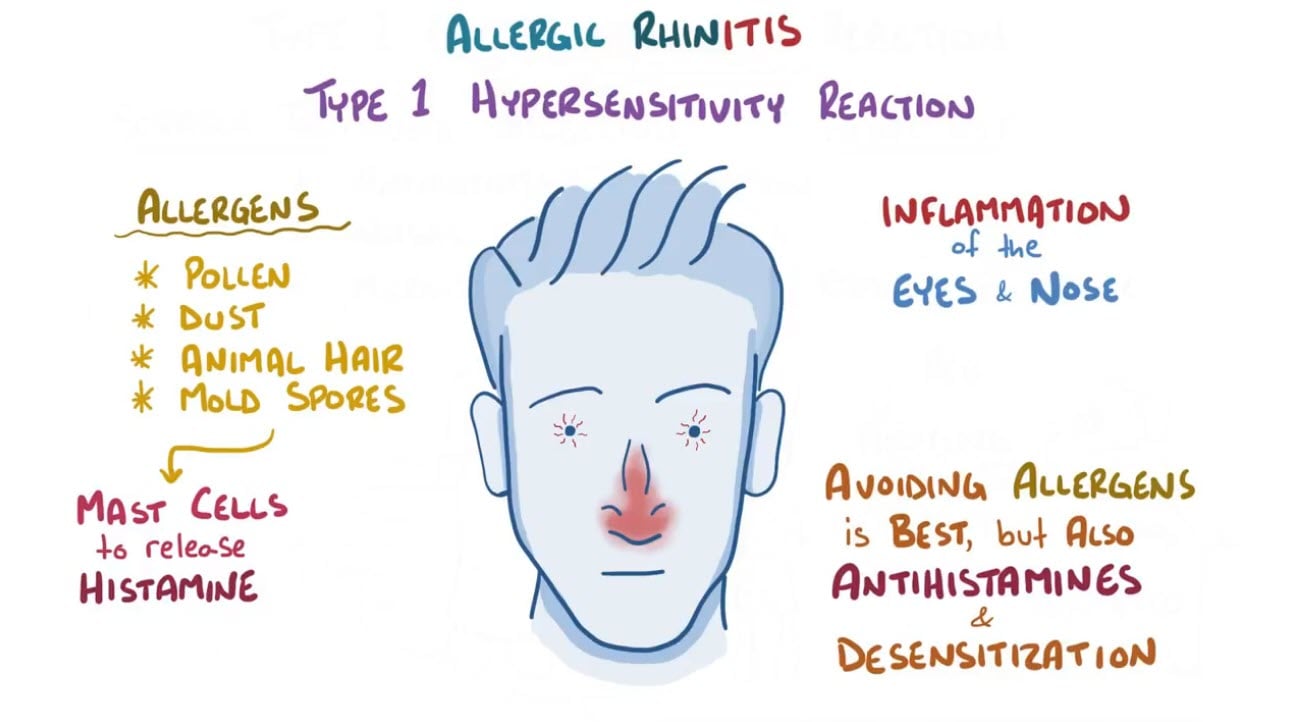
Rhinitis is inflammation and swelling of the mucous membrane of the nose, characterized by a runny nose and stuffiness - it can have allergic and nonallergic causes
- Allergic rhinitis is an immunoglobulin E (IgE)– mediated reactivity to airborne antigens (e.g., pollen, molds, danders, dust). It commonly occurs in people who have other atopic diseases (e.g., asthma, eczema, atopic dermatitis) and those with a family history
- Patients will present with boggy turbinates, allergic shiners (edematous, dark circles under eyes), and allergic salute: transverse nasal crease (from pushing up on the nose)
- Nonallergic rhinitis has symptoms similar to those of hay fever (allergic rhinitis) but with none of the usual evidence of an allergic reaction. The exact cause of nonallergic rhinitis is unknown
- Triggers of nonallergic rhinitis symptoms vary and can include certain odors or irritants in the air, weather changes, some medications, certain foods, and chronic health conditions.
Allergic rhinitis can almost always be diagnosed based on history alone
- Diagnostic testing is not routinely needed unless patients do not improve when treated empirically; for such patients, skin tests or an allergen-specific serum IgE test is done
Nonallergic perennial rhinitis is usually also diagnosed based on history
- Lack of clinical response to treatment for assumed allergic rhinitis and negative results on skin tests and/or an allergen-specific serum IgE test also suggests a nonallergic cause
Treatment of allergic rhinitis includes the avoidance of any known allergens and the use of antihistamines, cromolyn sodium, nasal or systemic corticosteroids, nasal saline drops or washes, and immunotherapy
- Intranasal decongestants are not to be used for more than 3-5 days
- Rhinitis medicamentosa is caused by the overzealous use of decongestant drops or sprays containing oxymetazoline or phenylephrine. This causes rebound congestion, which prompts increased use of the agent, creating a vicious cycle.
- To treat, discontinue the irritant. It may be quite uncomfortable for the patient; sometimes, the use of topical corticosteroids is warranted through the withdrawal period
- Even “nonsedating” antihistamines have a 15 percent sedation rate
Treatment of nonallergic rhinitis is similar and includes
- Avoidance of known triggers
- Topical intranasal glucocorticoids, topical antihistamines, and ipratropium have been shown to be beneficial
- Topical anticholinergic, ipratropium nasal spray (0.03%), two sprays in each nostril 3 times daily, is effective for cold-air-induced rhinitis
- Treatments effective for allergic rhinitis (oral antihistamines and cromolyn) may be added in mixed rhinitis
 Osmosis Osmosis |
|
 |
 Treatment includes avoidance of any known allergens and use of antihistamines, cromolyn sodium, nasal or systemic corticosteroids, nasal saline drops or washes, and immunotherapy.
Treatment includes avoidance of any known allergens and use of antihistamines, cromolyn sodium, nasal or systemic corticosteroids, nasal saline drops or washes, and immunotherapy.
Question 1 |
Azithromycin (Zithromax) Hint: Azithromycin is used to treat bacterial infections not allergic disorders. | |
Oral corticosteroids Hint: Oral corticosteroids are not typically first-line for seasonal allergic rhinitis unless the symptoms are severe and unresponsive to other treatments. | |
Intranasal corticosteroids | |
Pseudoephedrine Hint: Pseudoephedrine is a decongestant that may relieve the nasal congestion, but has no effect on the allergic response. |
Question 2 |
Ipratropium bromide Hint: Ipratropium bromide does not alleviate the sneezing and pruritus symptoms this patient is experiencing. | |
Montelukast Hint: Montelukast is less effective than intranasal steroids in the management of allergic rhinitis. | |
Immunotherapy | |
Cromolyn sodium Hint: Cromolyn sodium is much less potent than intranasal steroids and will likely not improve the patient's symptoms. |
Question 3 |
Clear rhinorrhea Hint: See D for explanation. | |
Erythematous pharynx Hint: See D for explanation. | |
Nasal flaring Hint: See D for explanation. | |
Pale nasal turbinates |
|
List |
References: Merck Manual · UpToDate



