NCCPA™ PANCE EENT Content Blueprint ⇒ ear disorders ⇒ middle ear
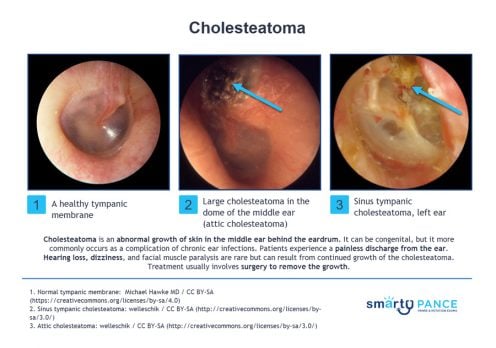
| Cholesteatoma | Patient will present as → a 43-year-old male with a “lifelong” history of chronic ear infections and episodic purulent drainage from his right ear canal. The patient is currently without symptoms. Examination of the ear shows a clear external canal, but the tympanic membrane is retracted, and there is a pocket of white material and an opacity of the pars flaccida. The Weber test lateralizes to the right, and Rinne shows air conduction > bone conduction on the left and bone conduction > air conduction on the right. Preparations are made to undergo a non-contrast computed tomography (CT) scan of the temporal bone. Cholesteatoma presents with painless otorrhea, brown/yellow discharge with a strong odor
DX: Diagnosis can be made with otoscopic visualization of granulation tissue
TX: Surgical removal |
| Otitis media (ReelDx) | ReelDx Virtual Rounds (Otitis media)Patient will present as → a 3-year-old previously healthy male is brought to your office by her mother. The mother reports the child has been crying and pulling at her right ear over the past 2 days and reports the patient has been febrile the past 24 hours. The patient’s past medical history is unremarkable, although the mother reports the patient had a “common cold” a week ago, which resolved without intervention. His temperature is 101.6 F, blood pressure is 100/70 mmHg, pulse is 120/min, and respirations are 22/min. The otoscopic exam is seen here. The clinical diagnosis of AOM requires 1) bulging of the tympanic membrane or 2) other signs of acute inflammation (e.g., marked erythema of the tympanic membrane, fever, ear pain) and middle ear effusion
DX: Otoscopic examination may reveal bulging, loss of landmarks, redness, injection of TM, and pus.
TX: First-line amoxicillin, second-line augmentin, macrolides if penicillin-allergic
|
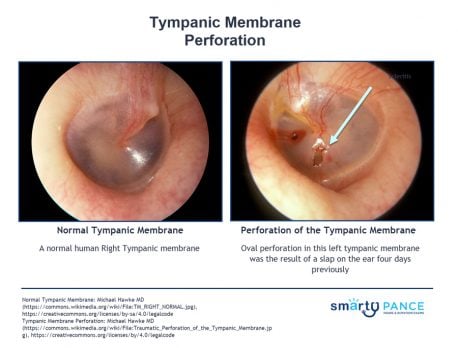
| Tympanic membrane perforation (ReelDx) | ReelDx Virtual Rounds (Tympanic membrane perforation)Patient will present as → a 9-month-old female with nasal congestion and cough is brought to your clinic by her mother, who reports that the child is very fussy, has been tugging at her right ear, and refuses to eat. On physical exam, you note copious green/yellow nasal discharge and right-sided otorrhea. An otoscopic exam reveals a significant amount of clear/white discharge obstructing your view. With careful examination, you are able to observe a ruptured right tympanic membrane. Tympanic membrane perforation presents with pain, otorrhea, and hearing loss/reduction Diagnosis is based on otoscopy TX: Most heal spontaneously, keep clean and dry, treat with antibiotics
|