To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
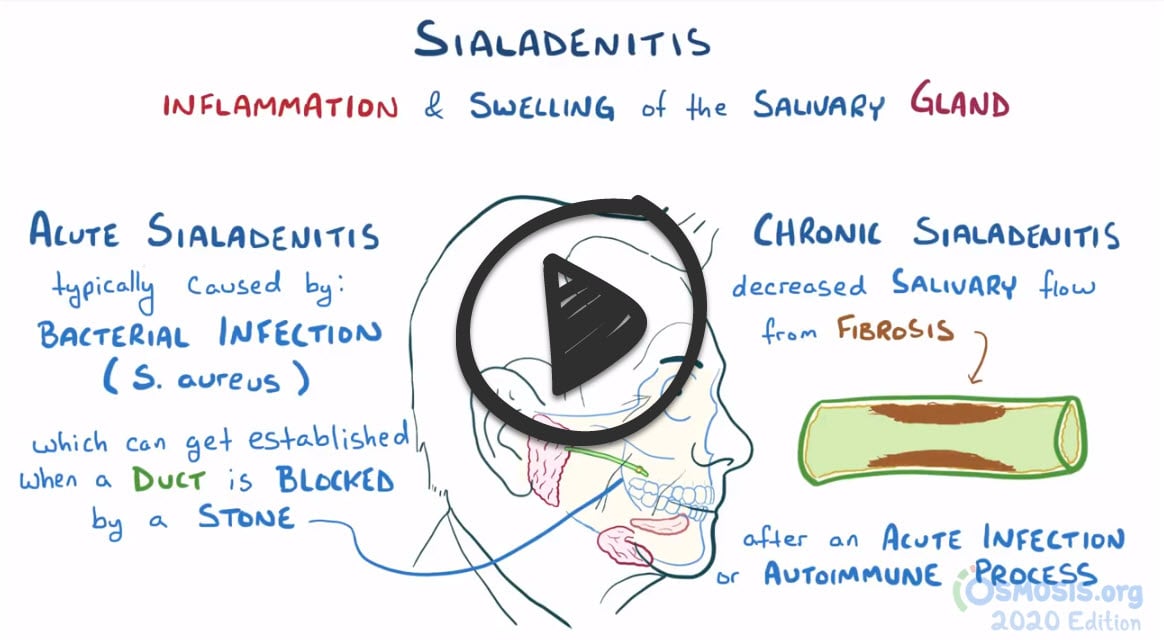
*** Sialadenitis is a bacterial infection of a salivary gland usually caused by sialolithiasis which is an obstructing stone in the salivary gland
I. Sialadenitis - is a bacterial infection of a salivary gland, usually due to an obstructing stone (sialolithiasis) or gland hyposecretion. Symptoms are swelling, pain, redness, and tenderness. Diagnosis is clinical. CT, ultrasonography, and MRI may help identify the cause. Treatment is with antibiotics.
- Bacterial infection of the parotid or submandibular salivary glands (often caused by prior sialolithiasis and blockage of salivary ducts).
- The most common pathogen is Staphylococcus Aureus
- Patients with Sjögren syndrome
- Treat with antibiotics (cephalosporin) and dilation of the salivary duct
- Increase salivary flow with sialogogues (have the patient suck on lemon drops)
II. Sialolithiasis - stones composed of Ca salts often obstruct salivary glands, causing pain, swelling, and sometimes infection. Diagnosis is made clinically or with CT, ultrasonography, or sialography. Treatment involves stone expression with saliva stimulants, manual manipulation, a probe, or surgery
- Salivary stones – most common in Wharton's duct (submandibular gland). Stenson's (parotid glands)
- Patients will present with postprandial salivary gland pain and swelling
- Treatment: Cephalosporin and dilation of the salivary gland duct, along with increased oral hydration and the use of sialogogues (as above)
- May require surgical marsupialization of the duct (removal of stone)
Sialadenitis:
- CT, ultrasonography, or MRI can confirm sialadenitis or abscess that is not obvious clinically, although MRI may miss an obstructing stone
- If pus can be expressed from the duct of the affected gland, it is sent for gram stain and culture
Sialolithiasis:
- Clinical diagnosis is usually adequate, but sometimes CT, ultrasonography, or sialography are needed
Sialadenitis
Antibiotics: Initial treatment is with IV antibiotics active against S. aureus
- With the increasing prevalence of methicillin-resistant S. aureus, especially among the elderly living in extended-care nursing facilities, vancomycin is often required.
- Local measures (e.g., sialagogues, warm compresses): Hydration, sialagogues (e.g., lemon juice, hard candy, or some other substance that triggers saliva flow), warm compresses, gland massage, and good oral hygiene are also important. Abscesses require drainage.
Sialolithiasis
- Many stones pass spontaneously or with the use of sialagogues (e.g., tart, hard candies, lemon drops, Xylitol-containing gum, or candy to increase salivary flow) and manual expression
- Some require endoscopic surgical removal or lithotripsy
Question 1 |
Sialogogues and warm compresses Hint: While sialogogues (agents that stimulate saliva production) and warm compresses can help improve salivary flow and provide symptomatic relief, they are adjunctive treatments and not sufficient as standalone therapy for acute bacterial sialadenitis, which requires antibiotic treatment. | |
Immediate surgical drainage Hint: Surgical drainage is not the first-line treatment for acute bacterial sialadenitis unless there is an abscess that fails to respond to antibiotics. Initial management should focus on antibiotics and supportive care. | |
Intravenous ampicillin-sulbactam | |
Oral hydration and analgesics Hint: Oral hydration and analgesics can provide supportive care and symptomatic relief but do not address the underlying bacterial infection. Antibiotics are necessary for treatment. | |
High-dose oral glucocorticoids Hint: Glucocorticoids are not indicated in the treatment of acute bacterial sialadenitis and may worsen the infection by suppressing the immune response. |
Question 2 |
A 75-year-old woman presents with acute onset of right-sided facial swelling and pain. She reports decreased appetite and a foul taste in her mouth. She is on multiple medications for hypertension and hyperlipidemia. Which of the following is the most likely predisposing factor to this patient's condition?
History of radiation therapy to the head and neck Hint: History of radiation therapy to the head and neck: Radiation therapy can cause salivary gland damage but usually presents as chronic dysfunction rather than acute infection. | |
Recent viral illness Hint: Viral infections can lead to parotitis (especially mumps) but typically presents with more bilateral gland involvement. | |
Autoimmune disease Hint: Sjogren Syndrome is associated with sialadenitis, but is more often chronic or recurrent rather than this acute picture. | |
Dehydration | |
Smoking Hint: While smoking can affect oral health, it's not directly associated with the development of acute sialadenitis. |
Question 3 |
Prescribe a course of broad-spectrum antibiotics Hint: Antibiotics are not indicated unless there is evidence of secondary bacterial infection, which is not suggested by the absence of purulent discharge and the patient's symptoms. | |
Advise increased hydration and sialogogues | |
Immediate surgical removal of the submandibular gland Hint: Surgical removal of the gland is considered only for recurrent or chronic cases that do not respond to conservative management or for stones that cannot be otherwise removed. It is not the first-line approach. | |
Ultrasound-guided fine-needle aspiration of the mass Hint: Fine-needle aspiration is not a standard treatment for sialolithiasis and is more appropriate for evaluating unknown masses or suspected neoplasms. | |
CT scan of the neck with contrast Hint: While imaging studies like ultrasound or non-contrast CT can be helpful in confirming the diagnosis and assessing the size and location of the stone, they are not the immediate next step before attempting conservative management. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture