2-year-old with fever, facial pain, dental caries, and facial edema
Patient will present as → a 25-year-old HIV-positive male with pain associated with his gums. He has also noted bleeding of his gums when he brushes his teeth. On physical exam, you observe a bright erythematous line along the gingival margin.
Gingivitis: Periodontitis is the most common cause of tooth loss. It occurs when chronic gingivitis (a result of bacterial plaque buildup) leads to loss of supporting bone around the tooth root.
- Symptoms include deepening of the gingival pockets between the teeth with the accumulation of calculus deposits. The gums soon lose their attachment to the tooth, and bone loss occurs. Bacteria accumulate in the gingival pockets and can lead to progression of the disease. Later in the course of the disease, the gums recede, and eventually, tooth loss occurs
- Treatment involves dental referral and, in severe cases, surgery. Regular dental visits twice yearly and proper brushing and flossing techniques help prevent plaque buildup
- Pt should be counseled about the increased risk of cardiovascular events
- Patients with HIV gingivitis present with a bright erythematous line along the gingival margin and complain of spontaneous bleeding
Gingival Hyperplasia
- An overgrowth of the gums to the point where it blocks the teeth, commonly caused by medications
- Phenytoin, CCBs, and Cyclosporine
Vincent's Angina “Trench Mouth”
- Necrotizing gingivitis: Characterized by the “punched-out” appearance of the gingival papillae. Caused by an overgrowth of oral flora. Occurs most often in children and young adults in developing nations. It mainly occurs in sub-Saharan Africa.
- Treatment: address malnutritions, Chlorhexidine gluconate (Peridex): 15 mL swish/spit BID, PO ABX.
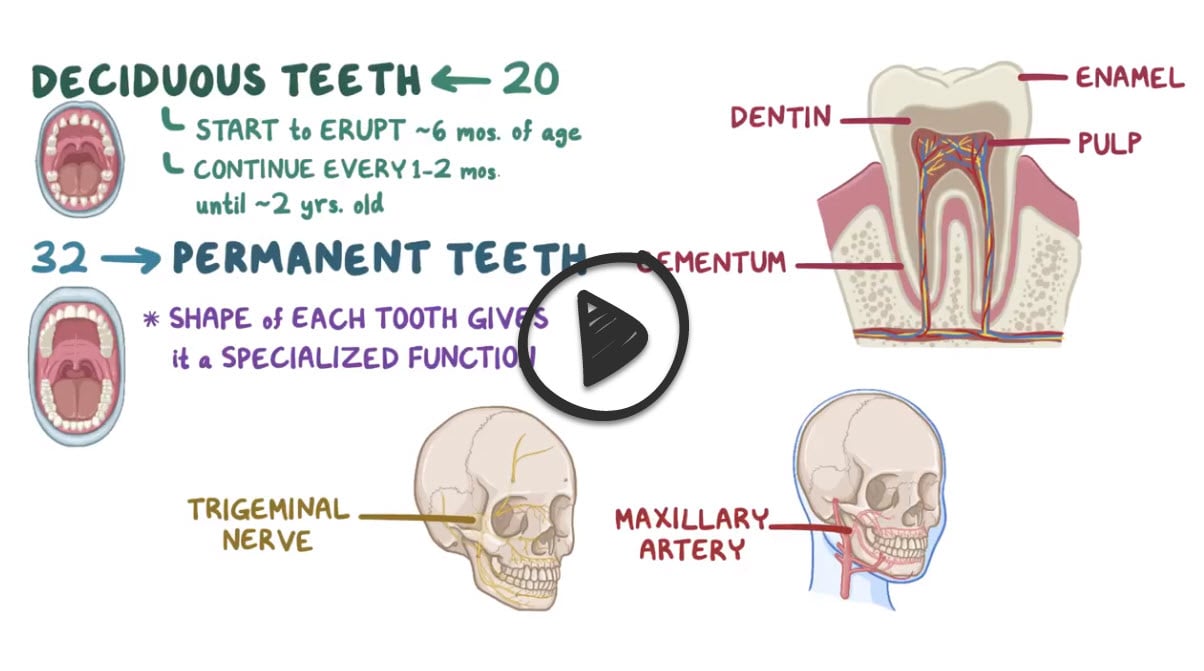
Dental abscess: Dental caries begin asymptomatically as a destructive process of the hard surface of the tooth. Over time, dental caries extend to the tooth pulp, which can lead to abscess formation. Abscesses are characterized by swelling, pain, and fever.
- Poor dental health is a risk factor for dental abscess or facial cellulitis
- Refer the complicated abscess to an oral surgeon for I&D
- Diagnose with a CT scan
- Treat: Ceftriaxone IM, followed by PO Augmenting or clindamycin
Question 1 |
dental abscess | |
halitosis Hint: Halitosis can be a sign of periodontal disease, oral abscess, xerostomia, esophageal stasis, sinusitis, lung abscess, systemic disease, or poor hygiene. It is not painful. Treatment is directed at the underlying cause. | |
mumps infection Hint: The prodrome of mumps includes fever, malaise, myalgia, and anorexia. Parotitis usually develops within the next 24 hours but may be delayed for as long as a week. It is generally bilateral. The submaxillary and sublingual glands are involved less often than the parotid. Swelling of the parotid obliterates the space between the ear lobe and angle of the mandible. The patient typically complains of earache and difficulty eating or talking. Stensen duct will be red and swollen.
| |
sialadenitis Hint: Acute bacterial sialadenitis typically affects the parotid or submandibular gland. There is swelling and pain which worsens with eating. There is tenderness and erythema of the duct opening, and massage may release purulent material. Ductal obstruction leads to salivary stasis and secondary infection; the most common organism is Staphylococcus aureus. |
Question 2 |
Periodontitis | |
Dental caries | |
Glossitis | |
Oropharyngeal cancer | |
Oropharyngeal candidiasis |
|
List |
References: Merck Manual · UpToDate


 Osmosis
Osmosis