Patient will present as → a 42-year-old white female complaining of a severely painful right eye. The pain is a constant, boring pain that worsens at night and in the early morning hours and radiates to the face and periorbital region. Additionally, she reports a headache, watering of the eye, and ocular redness.
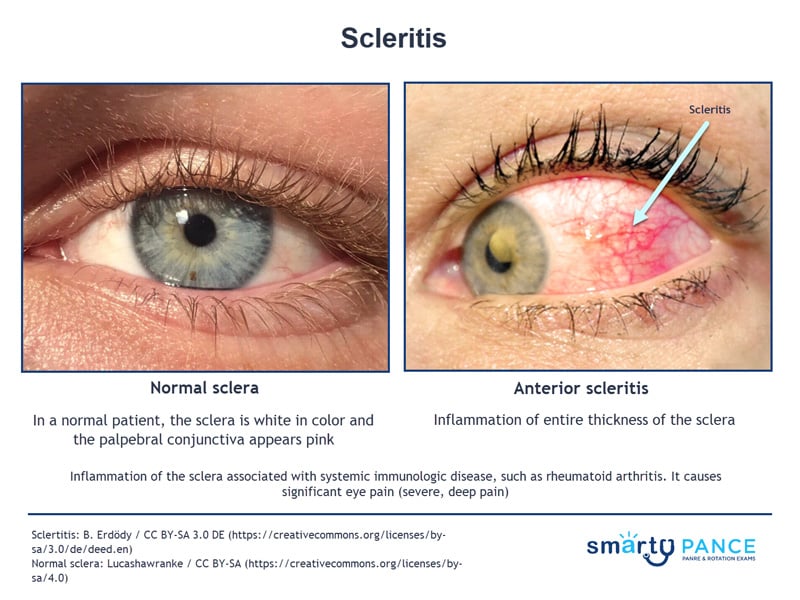
Inflammation of the sclera (the white outer coating of the eye) associated with systemic immunologic disease, such as rheumatoid arthritis
- It causes significant eye pain (severe, deep pain)
Refer the patient for prompt evaluation by an ophthalmologist
- Treatment involves topical and sometimes systemic corticosteroids
Question 1 |
A 69-year-old female with scleritis and has been taking 600 mg of ibuprofen three times per day. She presents for a follow-up and stated she had not had any improvement in her symptoms after 7 days. What is the next best treatment option at this time?
Prescribe oral prednisone 1 mg/kg/day for one month | |
Prescribe topical prednisolone acetate 1% four times per day for one week Hint: Topical steroids can be used as the first-line agent in addition to oral NSAID treatment. | |
Discontinue ibuprofen Hint: The patient has not responded to first-line treatment but requires additional treatment to manage inflammation. | |
Prescribe topical artificial tears four times per day Hint: Artificial tears do not manage inflammation. They may provide some relief to any ocular surface dryness present. |
Question 1 Explanation:
If there is no response with the first-line treatment of oral NSAIDs, then second-line treatment of oral steroids is indicated.
There is 1 question to complete.
References: Merck Manual · UpToDate