NCCPA™ PANCE EENT Content Blueprint ⇒ Oropharyngeal disorders
| Diseases of the teeth and gums (ReelDx) | ReelDx Virtual Rounds (Dental abscess)Patient will present as → a 25-year-old HIV-positive male with pain associated with his gums. He has also noted bleeding of his gums when he brushes his teeth. On physical exam, you observe a bright erythematous line along the gingival margin. (gingivitis)
|
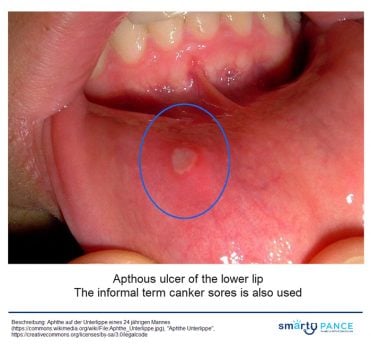
| Aphthous ulcers (ReelDx) | ReelDx Virtual Rounds (Aphthous ulcers)Patient will present as → a 22-year-old complaining of a painful sore for 2 days. He denies any alcohol or tobacco use and otherwise feels fine. The examination is significant for a 2-mm round ulceration with a yellow-gray center surrounded by a red halo on the left buccal mucosa Single or multiple small, shallow ulcers with a yellow-gray fibrinoid center with red halos DX: Diagnosis is made by history and clinical presentation
TX: viscous lidocaine 2–5% applied to ulcer QID after meals until healed |
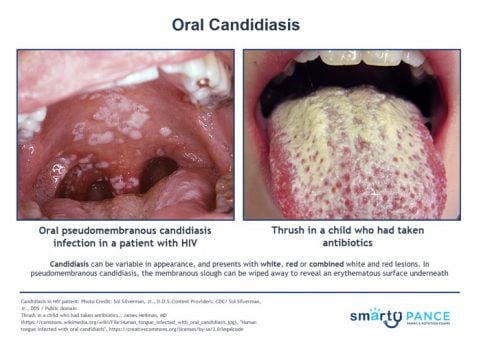
| Candidiasis (ReelDx) | ReelDx Virtual Rounds (Oral Candidiasis)Patient will present as → a 3-week-old infant with decreased appetite and a rash in her mouth. On physical exam, you note white plaques on her tongue that scrape off with a tongue depressor and bleed slightly. Potassium hydroxide (KOH) preparation of the scrapings demonstrates budding yeasts with hyphae. Immunocompromised, young patients
DX: Potassium Hydroxide (KOH) prep for diagnosis TX: Antifungals, which are available in several forms (i.e., ketoconazole or fluconazole orally, clotrimazole troches, nystatin liquid rinses) |
| Deep neck infection | Patient will present as → a 51-year-old male patient who underwent extraction of the mandibular right third molar. Seven days after the surgery, the patient developed facial edema, fever, intraoral purulent discharge, and extreme local pain. Infectious cavities in the right and left submandibular, pterygomandibular, and pharyngeal regions were observed on computed tomography scans. Deep neck space infections most commonly arise from a septic focus of the mandibular teeth, tonsils, parotid gland, deep cervical lymph nodes, middle ear, or sinuses
DX: Computed tomography (CT) is the imaging modality of choice for the diagnosis of deep neck space infection
TX: Antibiotics, aspiration, or surgical drainage should be performed  Minor trauma triggering cervicofacial necrotizing fasciitis from an odontogenic abscess. Image by Jain S, Nagpure PS, Singh R, Garg D - CC 2.0 |
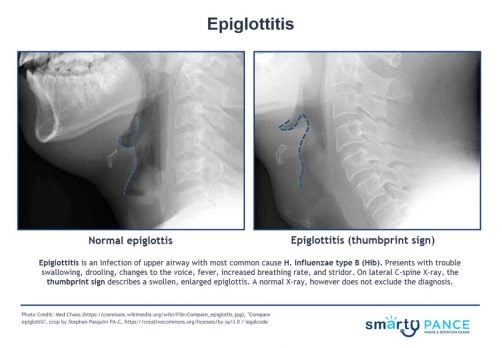
| Epiglottitis | Patient will present as → a 3-year-old who is brought into the emergency room by her parents. The child has had a high fever, sore throat, and stridor. She has a muffled voice and is sitting up on the stretcher, drooling while leaning forward with her neck extended. The patient’s parents are adamantly against vaccinations, claiming that they are a “government conspiracy.” You order a lateral neck x-ray, which shows a swollen epiglottis. The patient recovered following treatment with prednisone and ceftriaxone. Unvaccinated patient leaning forward, drooling, stridor, and distress (tripod position and muffled voice)
DX: Lateral radiograph: Thumbprint sign TX: Secure airway, admit, IV Ceftriaxone, and IV fluids |
| Oral herpes simplex (ReelDx) | ReelDx Virtual Rounds (Oral herpes simplex)Patient will present as → a 17-year-old female complaining of a painful rash on her cheek. She says that it has come and gone a few times before and that she usually can feel itching and a tingling discomfort before a break out of the lesions. On physical exam, you observe clusters of small, tense vesicles on an erythematous base. HSV type 1, vesicular lesions all in the same stage of development, a prodromal period of tingling discomfort or itching DX: Diagnosis is clinical; laboratory confirmation by culture, PCR, direct immunofluorescence, or serologic testing can be done TX: Symptomatic treatment with antipyretics and analgesia is recommended. IV hydration is sometimes needed in cases of decreased oral intake
|
| Laryngitis | Patient will present as → a 27-year-old mezzo-soprano who states that she developed acute hoarseness 2 days ago. Prior to that, she had a cold, the symptoms of which are improving. There is no history of smoking or other tobacco use. She is very worried as she has an upcoming performance 3 days from now. Almost always viral, hoarseness following a URI
DX: clinical diagnosis ⇒ laryngoscopy is required for symptoms persisting > 3 wk TX: Relax voice (vocal rest), supportive therapy
|
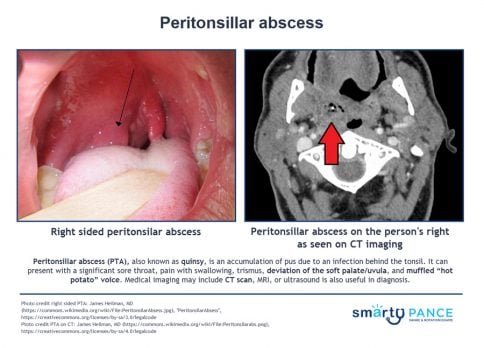
| Peritonsillar abscess (ReelDx) | ReelDx Virtual Rounds (Peritonsillar abscess)Patient will present as → a 19-year-old male who you are seeing for follow-up from the urgent care where he was seen 2 days earlier with a sore throat. The patient is febrile (102°F), has a muffled (hot potato) voice, and has extreme difficulty opening his mouth (trismus). He opens it just far enough for you to note uvular deviation. Presents with a severe sore throat, lateral uvula displacement, bulging tonsillar pillar
DX: Xray, CT, or ultrasound of the neck if the diagnosis is in doubt, particularly when the condition must be differentiated from a parapharyngeal infection or other deep neck infection
TX: Aspiration, incision and drainage, and/or antibiotics
|
| Pharyngitis (ReelDx) | ReelDx Virtual Rounds (Acute pharyngitis)Patient will present as → a 7-year-old boy is brought to his pediatrician for evaluation of a sore throat. The sore throat began 4 days ago and has progressively worsened. Associated symptoms include subjective fever, pain with swallowing, and fatigue. The patient denies cough or rhinorrhea. Vital signs are as follows: T 101.4 F, HR 88, BP 115/67, RR 14, and SpO2 99%. Physical examination is significant for purulent tonsillar exudate; no cervical lymphadenopathy is noted. Usually viral pharyngitis - adenovirus is the most common
DX: Centor Score for Strep Pharyngitis (MDcalc): 1. Absence of a cough, 2. exudates, 3. fever (> 100.4 F), 4. cervical lymphadenopathy
TX:
|
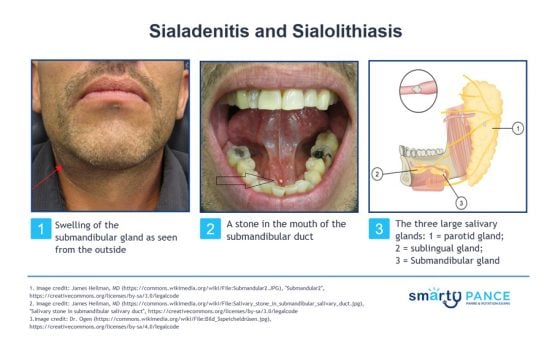
| Sialadenitis |
Patient will present as → a 39-year-old female complaining of episodic left-sided jaw pain and swelling. The symptoms are typically aggravated by eating or by the anticipation of eating. Over the last 2-days, the patient has been experiencing worsening pain, redness, and fever. On physical exam, the left salivary gland is exquisitely tender. High-resolution noncontrast computed tomography (CT) scanning reveals a left-sided salivary gland stone. Sialadenitis is a bacterial infection of a salivary gland usually caused by sialolithiasis, which is an obstructing stone in the salivary gland
DX: Sialadenitis:
Sialolithiasis:
TX: Sialadenitis Antibiotics: Initial treatment is with IV antibiotics active against S. aureus
Sialolithiasis
|
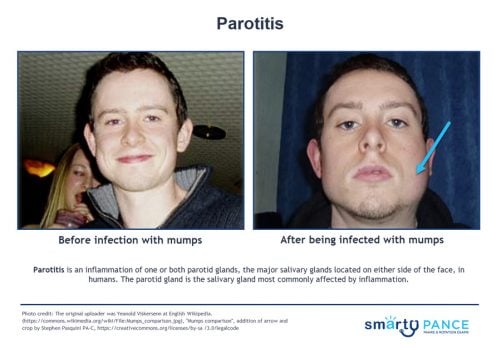
| Parotitis | ReelDx Virtual Rounds (Parotitis)Patient will present as → an 11-year-old boy with malaise and swelling of his face. He has no significant past medical history, but it is documented in his chart that his mother declined the recommended standard immunizations for children because of personal beliefs. Vital signs are stable, with the exception of a mild fever. In addition to the facial swelling, physical exam is also notable for swelling around the testes. There are no rashes. Parotitis is an inflammation of one or both parotid glands, the major salivary glands located on either side of the face, in humans
Causes:
Mumps parotitis
DX: often clinical
TX: Self-limiting - treat with hydration and rest
|
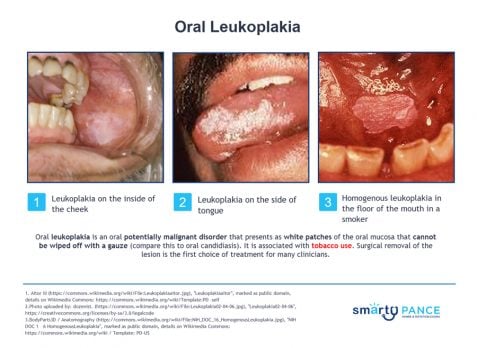
| Leukoplakia | Patient will present as → a 42-year-old male with symptoms of the flu. On social history, the patient describes drinking 2-3 beers per day as well as smoking 1 pack of cigarettes per day. He is noted on physical exam to have a white plaque-like lesion on the side of the tongue, which could not be scraped off with a tongue depressor. Oral leukoplakia is an oral potentially malignant disorder that presents as white patches of the oral mucosa that cannot be wiped off with gauze. (compare this to oral candidiasis)
DX: The diagnosis of leukoplakia is suspected in patients presenting with a white lesion of the oral mucosa that cannot be wiped off with gauze and that persists after eliminating potential etiologic factors, such as mechanical friction, for a six-week period
TX: For 2–3 circumscribed lesions, surgical excision
Patient will present as → a 42-year-old patient with AIDS presents with a grayish-white “corduroy-like” plaque on the lateral borders of her tongue that does not scrape off. Oral hairy leukoplakia is a separate disorder that is not premalignant. It is an Epstein-Barr virus-induced lesion that occurs almost entirely in HIV-infected patients
TX: Unlikely to progress to squamous cell carcinoma
"Thrush can be scraped off with a tongue depressor revealing inflamed mucosa underneath. Leukoplakia will remain intact when attempting to remove with a tongue depressor." |
Dental management of injuries to primary and permanent teeth
| Description | Primary dentition | Permanent dentition |
| Concussion/subluxation | Observe, soft foods for 1 week, dental radiograph to rule out root fracture | Observe, soft foods for 1 week, dental radiograph to rule out root fracture |
| Luxation | Reposition tooth or extract, do not splint | Dental radiograph, reposition tooth, splint for 4 weeks |
| Extrusion | Reposition tooth or extract, do not splint | Dental radiograph, reposition tooth, splint for 2 weeks |
| Intrusion | Dental radiograph, observe and allow to reerupt, extract if alveolar plate is compromised | Dental radiograph, observe and allow to reerupt, surgical or orthodontic repositioning, root canal treatment |
| Uncomplicated crown fracture | Restore tooth, smooth sharp edges, dental radiograph to rule out root fracture | Restore tooth, smooth sharp edges, radiograph to rule out root fracture |
| Complicated crown fracture | Dental radiograph, pulp treatment, restore or extract tooth, observe for infection | Dental radiograph, pulp treatment, restore tooth, observe for infection, may require root canal treatment |
| Root fracture | Dental radiograph, extract if root fracture is in middle or cervical third of root | Dental radiograph, splint, may require root canal treatment; if in cervical third, may need to extract |
| Avulsion | Do not replant, dental radiograph to rule out intrusion if tooth is not located | Do not handle the root, replant within 30 min or place in recommended transport medium (balanced salt solution, cold milk); dental radiograph, replant and splint as soon as possible; systemic antibiotics, soft diet, chlorhexidine, close follow-up |