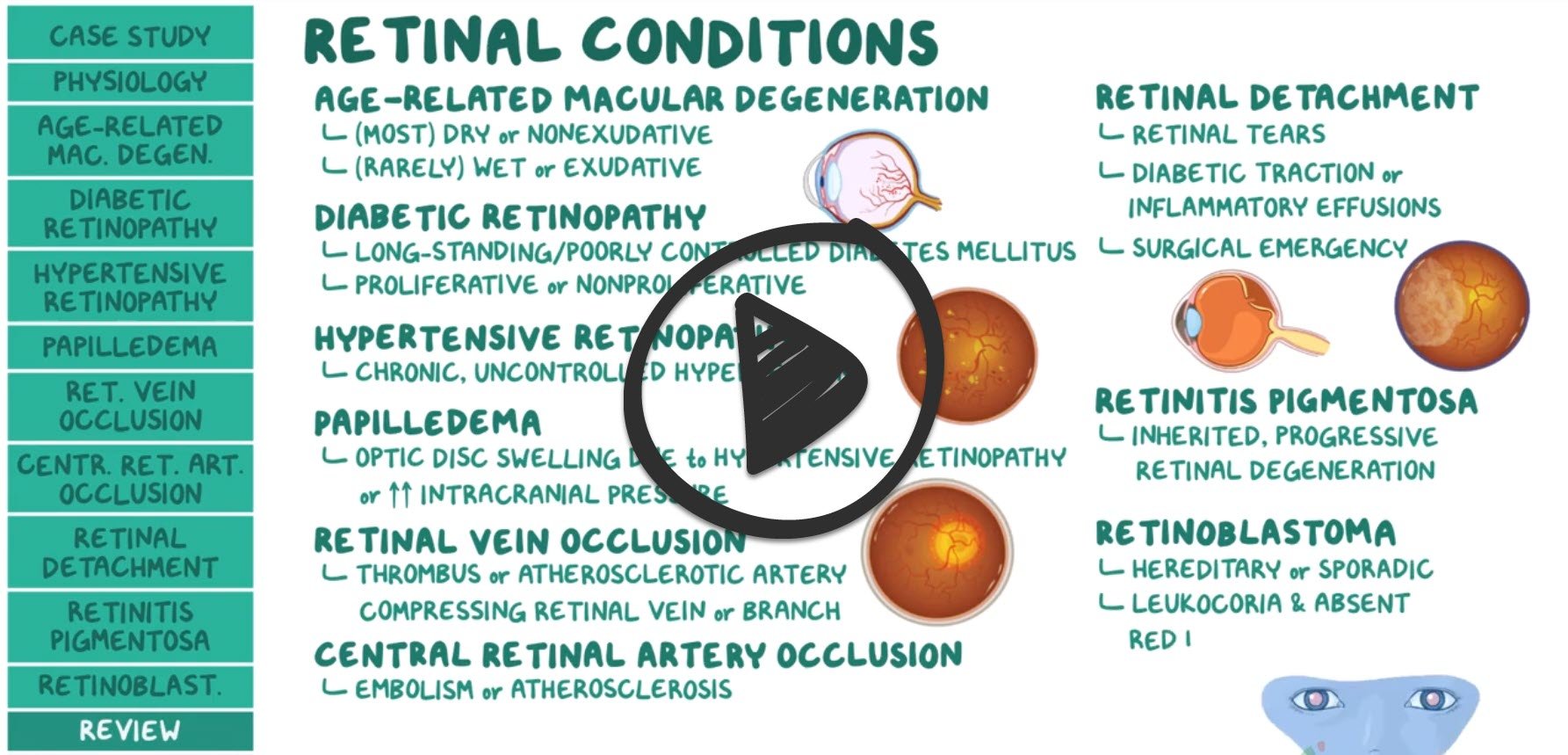
Retinal disorders (PEARLS)
NCCPA™ PANCE EENT Content Blueprint eye disorders ⇒ retinal disorders
 Osmosis Osmosis |
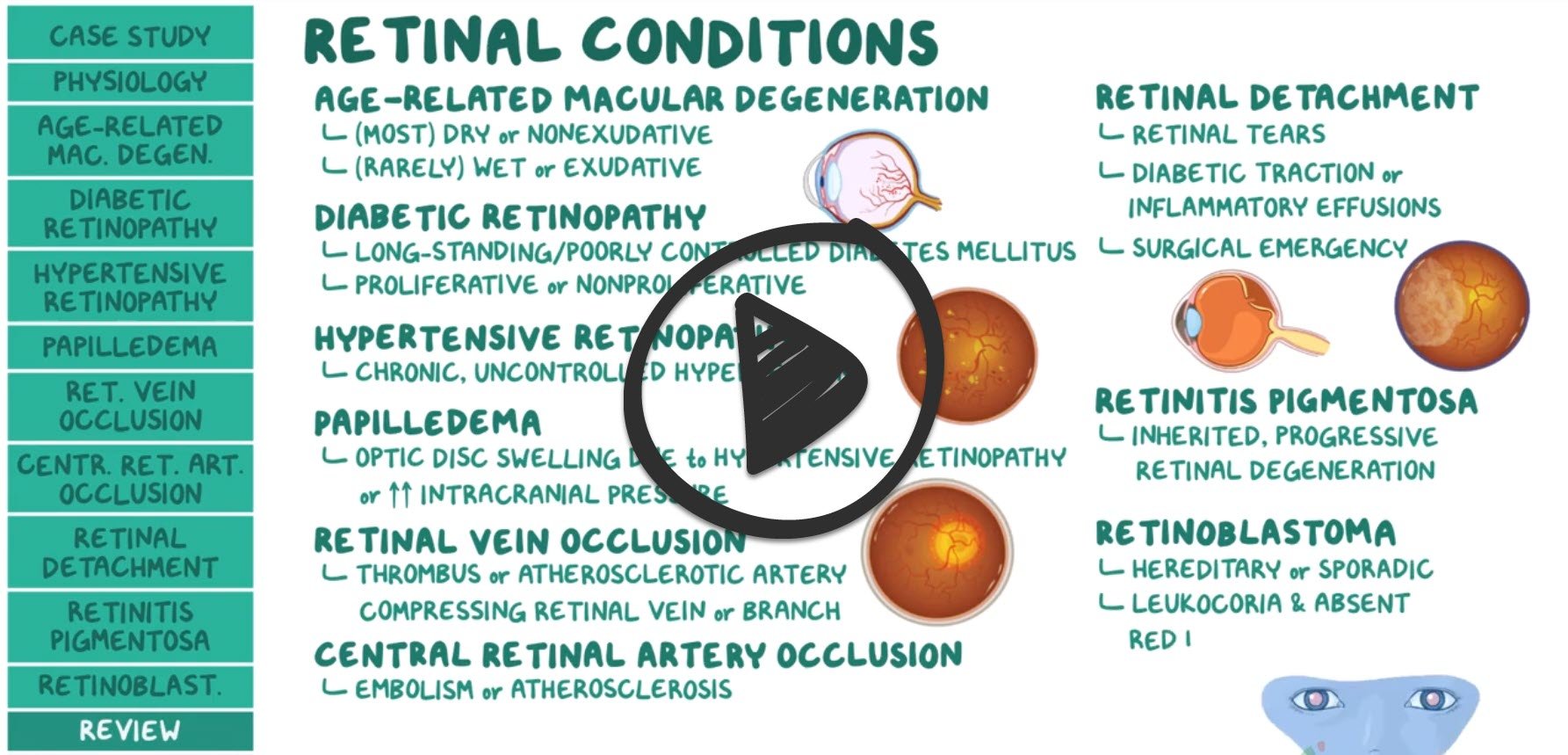 |
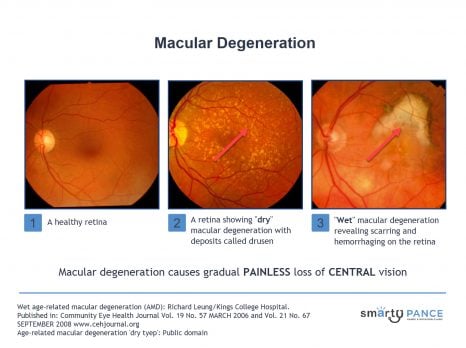
| Macular degeneration |
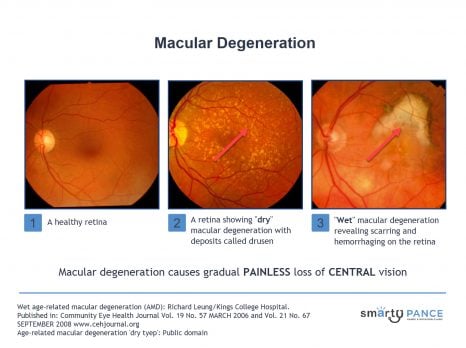
Patient will present as → a 62-year-old male who arrives for his follow-up visit for chronic central visual loss. He describes a phenomenon of wavy or distorted vision that has deteriorated rather quickly. The patient is frustrated because he “just can’t drive anymore,” and he is “having difficulty seeing words when he reads.” When looking at a specific region of the Amsler grid, he reports a dark “spot” in the center, with bent lines. On the fundoscopic exam, you note areas of retinal depigmentation along with the presence of yellow retinal deposits. Gradual painless loss of central vision. The macula is responsible for central visual acuity, which is why macular degeneration causes gradual central field loss.
DX: funduscopic findings are diagnostic; color photographs, fluorescein angiography, and optical coherence tomography assist in confirming the diagnosis and in directing treatment.
TX:
Wet age-related macular degeneration
- VEGF inhibitors (e.g., bevacizumab)
- Photodynamic therapy
- Zinc and antioxidant vitamins
Dry age-related macular degeneration
- Zinc and antioxidant vitamin
|
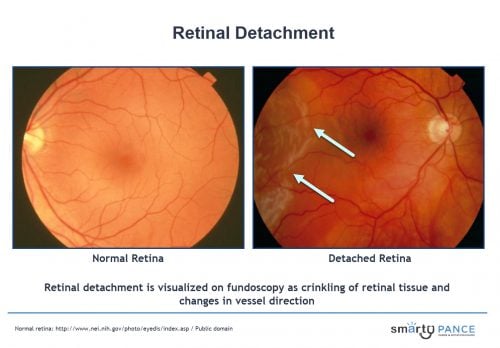
| Retinal detachment |
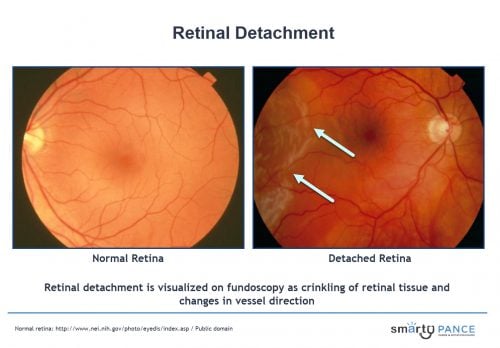
Patient will present as → a 65-year-old man complaining of a sudden unilateral vision loss, which he describes as a “curtain or dark cloud lowering over my eye.” This was preceded by small moving flashing lights and floaters. The fundoscopic exam reveals a detached superior retina. Separation of the retina from the pigmented epithelial layer causing the detached tissue to appear as a flap in the vitreous humor
- Can occur spontaneously or secondary to trauma or extreme myopia
- Vertical curtain coming down (curtain of darkness) across the field of vision may sense floaters or flashes at the onset, loss of vision over several hours (acute and painless)
- Myopia (nearsightedness) is a risk factor for the development of retinal detachment
- Retinal detachment usually presents with defects in the peripheral visual field
DX: is by fundoscopy
- Retinal detachment is visualized on fundoscopy as crinkling of retinal tissue and changes in vessel direction
- Ultrasonography may help determine the presence and type of retinal detachment if it cannot be seen with funduscopy
TX: Retinal detachment is an ophthalmologic emergency
- Stay supine (lying face upward) with head turned towards the side of the detached retina
- Consult ophthalmologist
- Pneumatic retinopexy is a procedure for the management of retinal detachment that involves cryoretinopexy followed by injection of an air bubble in the vitreous
|
| Retinopathy |
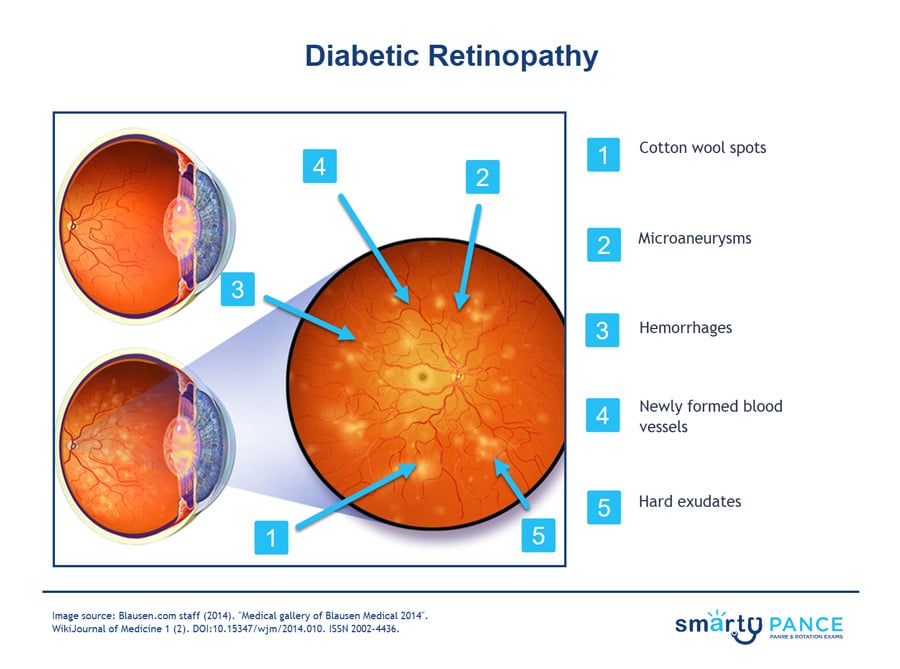
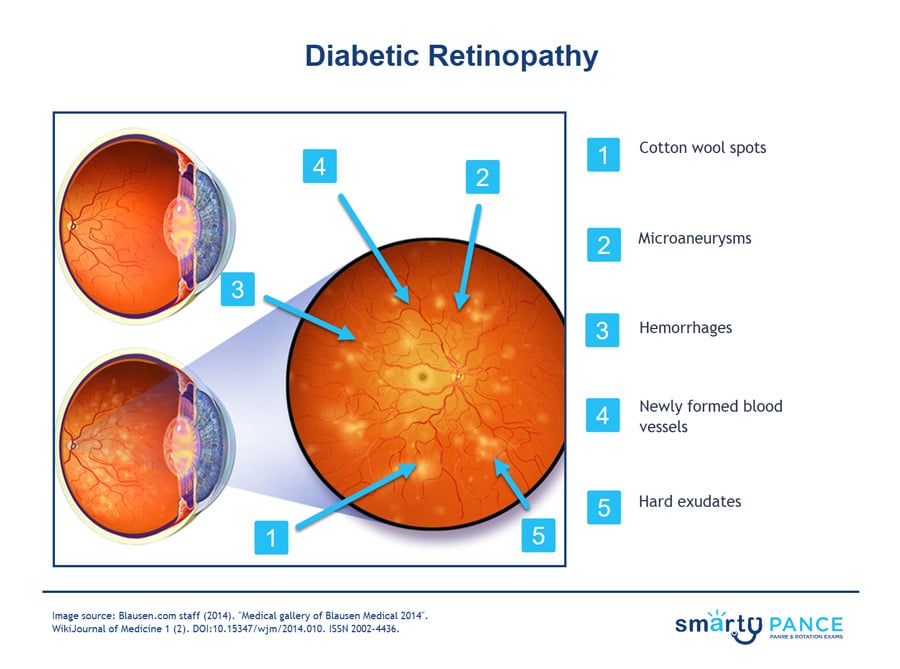
Patient will present as → a 65-year-old woman with a 10-year history of type 2 diabetes mellitus presents for a routine eye examination. She reports no visual symptoms. Her last eye examination was 2 years ago. On fundoscopic examination, you note microaneurysms, dot and blot hemorrhages, and hard exudates in both eyes. There is no evidence of neovascularization or vitreous hemorrhage. Caused by systemic disorders, including diabetes, hypertension, preeclampsia-eclampsia, blood dyscrasias, and HIV disease -may affect the retina
- Diabetic retinopathy falls into two main classes: nonproliferative (early) and proliferative (late, advanced)
- Prolonged hyperglycemia causes basement membrane thickening, decreased pericytes (hyperproliferation), microaneurysms, and neovascularization
- Leading cause of blindness in adults
Hypertensive retinopathy is retinal damage caused by high blood pressure.
- In the early stages, there may be no symptoms at all
- As the condition progresses, patients may experience blurred vision, floaters, and difficulty seeing in low light
- In severe cases, hypertensive retinopathy can lead to blindness
Nonproliferative type (an early form of the disease)
- Non-proliferative diabetic retinopathy (NPDR) is the early stage of the disease in which symptoms will be mild or nonexistent
- In NPDR, the blood vessels in the retina are weakened
- Fundoscopy:
- Microaneurysms: Tiny bulges in the walls of retinal blood vessels.
- Hard exudates: Yellowish deposits on the retina that are caused by leakage of blood plasma and lipids.
- Cotton wool spots: White or fluffy spots on the retina that are caused by damage to nerve fibers.
- Blot and dot hemorrhages: Small, round hemorrhages on the retina.
- Venous dilation: Widening of the retinal veins.
Proliferative type (most severe, abnormal blood vessel growth)
- Proliferative diabetic retinopathy (PDR) is the more advanced form of the disease
- At this stage, circulation problems deprive the retina of oxygen. As a result, new, fragile blood vessels can begin to grow in the retina and into the vitreous. The new blood vessels may leak blood into the vitreous, clouding vision
- Fundoscopic exam (abnormal growth of vessels) neovascularization
TX: control of blood glucose and BP
- Ocular treatments: retinal laser photocoagulation, intravitreal injection of antivascular endothelial growth factor drugs (eg, ranibizumab, bevacizumab), intraocular corticosteroids, vitrectomy, or a combination
- If diabetic, get yearly dilated ophthalmoscopic examination
|
Back to PANCE Blueprint EENT (7%)
 Osmosis
Osmosis