67 y/o male with acute onset, unilateral visual changes
Patient will present as → a 65-year-old man complaining of a sudden unilateral vision loss, which he describes as a "curtain or dark cloud lowering over my eye." This was preceded by small moving flashing lights and floaters. The fundoscopic exam reveals a detached superior retina.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Retinal detachment is a separation of the neurosensory retina from the underlying retinal pigment epithelium. The most common cause is a retinal tear (rhegmatogenous detachment)
- If a patient complains of the new onset of floaters or flashes of light, the patient should undergo a dilated eye exam to rule out a retinal tear or retinal detachment
- Classically described as "a curtain or dark cloud lowering over my eye"
- Sudden and painless
- Often is spontaneous, but may have an underlying cause – for example, recent cataract surgery
- Myopia (nearsightedness) is a risk factor for the development of retinal detachment
- Retinal detachment usually presents with defects in the peripheral visual field
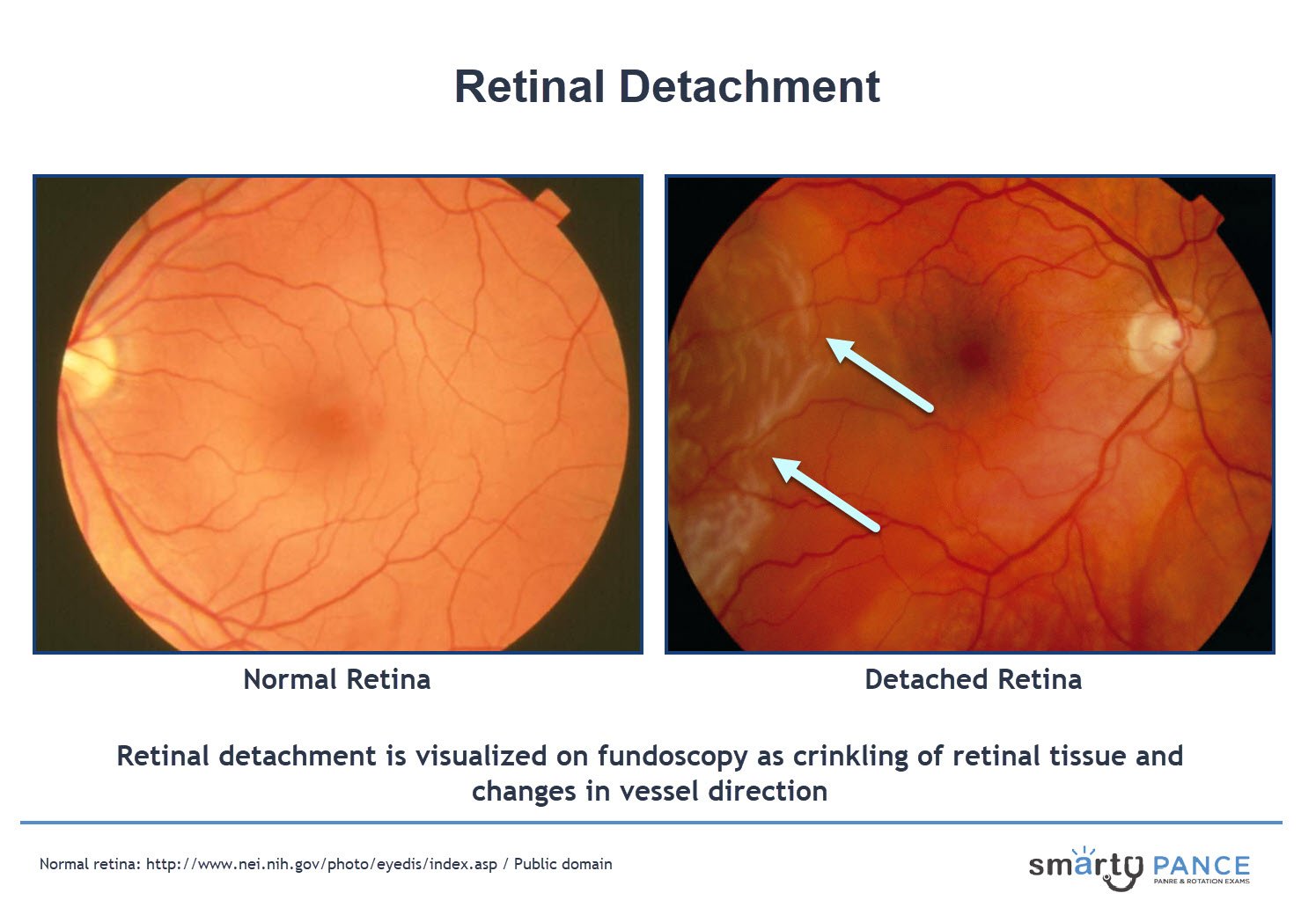
Diagnosis is by fundoscopy
- Retinal detachment is visualized on fundoscopy as an irregular elevation of the retina with crinkling of retinal tissue and changes in vessel direction
- Ultrasonography may help determine the presence and type of retinal detachment if it cannot be seen with funduscopy
- If there is no obvious vitreous abnormality, consider CT/MRI and/or neurologic consultation as well
Retinal detachment is an ophthalmologic emergency
- Stay supine (lying face upward) with head turned towards the side of the detached retina
- Pneumatic retinopexy is a procedure for the management of retinal detachment that involves cryoretinopexy followed by injection of an air bubble in the vitreous
A detached retina is caused by an accumulation of fluid leading to the separation of the sensory retina and underlying pigment epithelium. Symptoms may include flashes of light, floaters, and a curtain-like shadow. Interventions for retinal detachment include promoting bed rest, avoiding vigorous activity, wearing an eye patch, and preparing for immediate surgical repair.
Play Video + QuizQuestion 1 |
Central retinal vein occlusion Hint: Central retinal vein occlusion causes painless, variable loss of vision. Exam shows retinal hemorrhages in all quadrants and edema of the optic disk. | |
Retinal artery occlusion Hint: Retinal artery occlusion presents with sudden, painless loss of vision. Exam shows pale retina with normal macula, seen as a cherry-red spot. | |
Retinal detachment | |
Hyphema Hint: Hyphema is usually associated with trauma, and is a collection of blood in the anterior chamber |
Question 2 |
Central retinal vein occlusion Hint: Central retinal vein occlusion is characterized by sudden monocular visual loss on examination there would be disc swelling, venous engorgement, cotton-wool spots, and diffuse retinal hemorrhages. | |
Acute angle-closure glaucoma Hint: Acute angle-closure glaucoma is characterized by pain and blurred vision. On examination the eye is red, the cornea is steamy, and the pupil is moderately dilated and nonreactive to light. | |
Acute nongranulomatous anterior uveitis Hint: Acute nongranulomatous anterior uveitis presents with acute unilateral eye pain, redness, photophobia, and vision loss. | |
Serous retinal detachment |
|
List |
References: Merck Manual · UpToDate