The NCCPA™ EENT PANCE and PANRE Content Blueprint covers 55 topics - this is a high-yield review summarizing all topics from the blueprint, including a combined flashcard set.
| Disorders of the Eye (PEARLS) | |
| Blepharitis | Eyelid changes: crusting, scaling, red-rimming of eyelid and eyelash flaking along with dry eyes and associated seborrhea and rosacea |
| Blowout fracture (ReelDx) | History of blunt trauma, eyelid swelling, decreased visual acuity, enophthalmos (sunken eye), anesthesia/paresthesia in the gums, upper lips and cheek due to damage to the infraorbital nerve |
| Cataract | Blurred vision over months or years, halos around lights. Clouding of the Lens (versus clouding of cornea = glaucoma) |
| Chalazion | A chalazion is a painless (non-infectious) granuloma of the internal meibomian sebaceous gland, painless "cold" lid nodule, versus hordeolum, which is a painful infectious "hot" nodule |
| Conjunctivitis (ReelDx) | Viral: copious watery discharge, scant mucoid discharge
Bacterial: Pt will present with purulent (yellow) discharge, crusting, usually worse in the morning Allergic: red eyes, itching and tearing, usually bilateral, cobblestone mucosa on the inner/upper eyelid Gonococcal: copious purulent discharge, in a patient who is not responding to conventional treatment Chlamydial - Giemsa stain - inclusion body, scant mucopurulent discharge |
| Corneal abrasion (ReelDx) | Sudden onset of eye pain, photophobia, tearing, foreign body sensation, blurring of vision, and/or conjunctival injection, fluorescein dye - increased absorption in devoid area, antibiotic eye ointment, NO PATCHING! |
| Corneal ulcer | Contact lens wearers, caused by deep infection in the cornea by bacteria, viruses or fungi, Fluorescein stain - round "ulceration" versus "dendritic" pattern like herpes |
| Dacryoadenitis | Dacryoadenitis is inflammation of the nasolacrimal duct or the nasolacrimal gland (supratemporal)
Dacryocystitis is infectious obstruction of nasolacrimal duct (inferomedial region) |
| Ectropion | Ectropion (eversion of the eyelid) occurs when the eyelid turns outward exposing the palpebral conjunctiva, conjunctiva will appear red from air exposure and inflammation |
| Entropion | Entropion (inversion of an eyelid) is most commonly caused by age-related tissue relaxation, surgical correction is definitive |
| Ocular Foreign body | Metallic foreign bodies may leave a rust ring, irrigation, immediate surgical removal by an ophthalmologist |
| Glaucoma | Open angle glaucoma - peripheral to central, gradual visual loss (versus macular degeneration which is central loss)
Acute angle closure glaucoma - classic triad: injected conjunctiva, cloudy or “steamy” cornea, and fixed dilated pupil, this is an ophthalmic emergency. |
| Hordeolum (ReelDx) | Painful, warm (hot), swollen red lump on the eyelid (different from a chalazion which is painless) Think “H” for Hot = Hordeolum |
| Hyphema (ReelDx) | Collection of blood inside the front part of the eye (called the anterior chamber, between the cornea and the iris). The blood may cover part or all of the iris (the colored part of the eye) and the pupil, and may partly or totally block vision in that eye |
| Macular degeneration | Gradual central field loss, the macula is responsible for central visual acuity which is why macular degeneration causes gradual central field loss, Dry macular degeneration (85% of cases): Atrophic changes with age – slow gradual breakdown of the macula, with Dry = DRUSEN = yellow retinal deposits. |
| Optic neuritis (ReelDx) | Acute inflammation and demyelination of the optic nerve leads to acute monocular vision loss and pain in the affected eye, Multiple sclerosis is the most common cause |
| Orbital cellulitis | Decreased extraocular movement, pain with movement of the eye and proptosis, signs of infection |
| Papilledema | Optic disc swelling that is caused by increased intracranial pressure. The swelling is usually bilateral and can occur over a period of hours to weeks |
| Pterygium (ReelDx) | Elevated, superficial, fleshy, triangular-shaped “growing” fibrovascular mass (most common in inner corner/nasal side of the eye) |
| Retinal detachment | Flashers, floaters, asymmetric red reflex, described as a curtain or dark cloud coming across the field of vision, Keep patient supine (lying face upward) |
| Retinal vascular occlusion | Sudden, painless, unilateral, and usually severe vision loss (Amaurosis fugax), ruptured plaque from same sided (ipsilateral) carotid artery. Look for the cherry red spot |
| Retinopathy | Most common cause of new, permanent vision loss and/or blindness in 25–74-year-old, most common is diabetic retinopathy, Cotton wool spots, hard exudates, blot and dot hemorrhages, neovascularization, flame hemorrhages, A/V "nicking" |
| Strabismus (ReelDx) | Strabismus is defined as any form of ocular misalignment, The cover/uncover test is used to diagnose strabismus, Exotropia: out-turning of eyes, Esotropia: in-turning of eyes |
| Ear Disorders (PEARLS) | |
| Acute/chronic otitis media (ReelDx) | Limited mobility of the TM with pneumotoscopy, streptococcus pneumoniae 25%, Haemophilus influenzae 20%, first line Amoxicillin, second line Augmentin, macrolides if pen allergic |
| Acoustic neuroma | Benign tumor of the Schwann cells (the cells which produce myelin sheath) – most commonly affect the vestibular division of the 8'th cranial nerve. Slowly progressive unilateral hearing loss +/- vertigo, stereotactic radiation therapy |
| Barotrauma | Common injury in divers or while flying, sudden onset of pain that may resolve with a "pop" |
| Cholesteatoma | Painless otorrhea, brown/yellow discharge with strong odor, caused by chronic eustachian tube dysfunction which results in chronic negative pressure and inverts part of the TM causing granulation tissue that over time, erodes the ossicles and leads to conductive hearing loss |
| Dysfunction of the eustachian tube | Ear fullness, popping of ears, underwater feeling, intermittent sharp ear pain, fluctuating conductive hearing loss, tinnitus. All children < 7 years old have some ET dysfunction (based on the angle of the eustachian tube) will resolve with age |
| Foreign body in ear (ReelDx) | Insects must be immobilized prior to removal. Drown insects with mineral oil or viscous lidocaine before attempting removal, after irrigation, if the child is uncomfortable, consider treating with topical pain agents such as benzocaine-antipyrine |
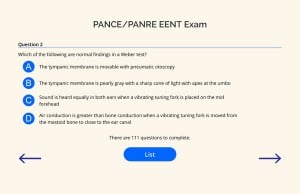
| Hearing impairment | Weber test: Tuning fork is placed on center of the head and see if sound lateralizes - lateralizes to bad ear with conductive hearing loss and lateralizes to better ear with sensorineural hearing loss
Rinne test: Tuning fork placed on mastoid and then up to the ear (should continue to hear) conductive hearing loss if bone > air, sensorineural hearing loss if air > bone |
| Hematoma of the external ear | Shearing forces to the anterior auricle lead to separation of the anterior auricle perichondrium from the underlying cartilage. May result in thickening of cartilage (cauliflower ear) if not treated promptly! |
| Labyrinthitis | Acute onset, vertigo + hearing loss of several days to a week, absence of neurologic deficits, try meclizine (No Tinnitus like Meniere disease) |
| Mastoiditis (ReelDx) | Fever, otalgia, pain & erythema posterior to the ear, and forward displacement of the external ear (ReelDx video), Treat with admission and IV antibiotics, drainage of middle ear fluid |
| Meniere disease | Classic triad of low frequency hearing loss, tinnitus with aural (ear) fullness and vertigo, treat with low salt diet, diuretics (HCTZ + triamterene) to reduce aural pressure |
| Otitis externa | Edema with cheesy white discharge, palpation of the targus is painful, malignant otitis externa is commonly seen in diabetics – caused by pseudomonas tx with fluoroquinolone |
| Tinnitus | Perceived sensation of sound in the absence of an external acoustic stimulus; often described as a ringing, hissing, buzzing, or whooshing. 90% is associated with sensorineural hearing loss – caused by loud noise, presbycusis, medications (Aspirin, Antibiotics, Aminoglycosides, loop diuretics and CCBs), Meniere's disease, acoustic neuroma. |
| Tympanic membrane perforation (ReelDx) | Pain, otorrhea and hearing loss/reduction, treat with antibiotics, the only class of antibiotics that are non-ototoxic are Floxins drops and should be used if you are going to be prescribing drops with a perforated TM |
| Vertigo (ReelDx) | Vertigo + Syncope = vertebral basilar insufficiency
Benign Positional Vertigo: Dix Hallpike for diagnosis. Treat using Epley's maneuver - pt. lays down and head is turned in a certain manner right to left Central vertigo: + Romberg Sign |
| Nose and Sinus Disorders (PEARLS) | |
| Acute and chronic sinusitis (ReelDx) | Sinus pain/pressure (worse with bending down and leaning forward), Plainview X-ray (waters view) is a good initial screening, CT is the GOLD STANDARD, Indications for antibiotics in rhinosinusitis include duration of symptoms >10 days without improvement, Augmentin 875 BID, kids Amoxicillin x 10-14 days |
| Allergic rhinitis (ReelDx) | Boggy turbinates, allergic shiners, IgE mediated mast cell histamine release, intranasal decongestants not to be used more than 3-5 days may cause rhinitis medicamentosa |
| Epistaxis (ReelDx) | Kiesselbach's Plexus or Little's Area is the most common site for anterior bleeds, sphenopalatine artery is generally the source of severe posterior nosebleed, direct pressure for 15 minutes, posterior balloon packing is used to treat posterior epistaxis |
| Nasal foreign body (ReelDx) | Purulent, foul-smelling nasal discharge |
| Nasal polyps | Teardrop-shaped growths that form in the nose or sinuses, Samter's triad: Asthma, Aspirin sensitivity and nasal polyps |
| Mouth and Throat Disorders (PEARLS) | |
| Acute pharyngitis (ReelDx) | Mononucleosis - atypical lymphocytes, + heterophile agglutination test (monospot). Taking antibiotics such as amoxicillin or ampicillin may cause a rash
Consider gonorrhea pharyngitis in patients with recent sexual encounters, or with non-resolving pharyngitis Fungal cause of pharyngitis in patients using inhaled steroids Throat culture is GOLD STANDARD, Penicillin is first line for Strep. Throat, Azithromycin if Pen allergic. |
| Aphthous ulcers (ReelDx) | Single or multiple small, shallow ulcers with yellow gray fibrinoid center with red halos, Biopsy should be considered for ulcers lasting more than 3 wks., viscous lidocaine 2–5%: applied to ulcer QID after meals until healed |
| Diseases of the teeth and gums (ReelDx) | Gingivitis: Pt should be counseled about increases risk for cardiovascular events
Gingival Hyperplasia: Overgrowing of gums so that it blocks the teeth, commonly caused by medications. Phenytoin, CCB's and Cyclosporine Vincent's Angina: “Trench Mouth” Necrotizing gingivitis: Characterized by the “punched-out” appearance of the gingival papillae Dental abscess: Poor dental health is a risk factor for dental abscess or facial cellulitis, refer the complicated abscess to an oral surgeon for I&D. |
| Epiglottitis | Drooling + dysphagia and distress (tripod position, muffled voice), H. influenza type B (Hib)
|
| Laryngitis | Almost always viral, consider squamous cell carcinoma if hoarseness persists > 2 weeks, history of ETOH and or smoking, Laryngoscopy is required for symptoms persisting > 3 wk. |
| Oral Candidiasis (ReelDx) | White plaques on oral mucous membranes that scrape off and may bleed when scraped (candidiasis can "come off"), Potassium Hydroxide (KOH) prep for diagnosis |
| Oral herpes simplex (ReelDx) | Prodromal period (typically < 6 h in recurrent HSV-1) of tingling discomfort or itching, treat with acyclovir |
| Oral leukoplakia | White plaque-like lesions on the side of the tongue that cannot be rubbed off |
| Peritonsillar abscess (ReelDx) | Hot potato (muffled) voice and deviation of the uvula to one side |
| Parotitis (ReelDx) | Caused by Paramyxovirus (Mumps), in adult males look for an associated orchitis. |
| Sialadenitis | Sialadenitis is a bacterial infection of a salivary gland usually caused by salolithiaisis which is an obstructing stone in the salivary gland
Diagnose with CT, ultrasonography, or MRI: CT, ultrasonography, and MRI can confirm sialadenitis or abscess that is not obvious clinically, although MRI may miss an obstructing stone. If pus can be expressed from the duct of the affected gland, it is sent for Gram stain and culture. |
EENT Benign and Malignant Neoplasms
|
|