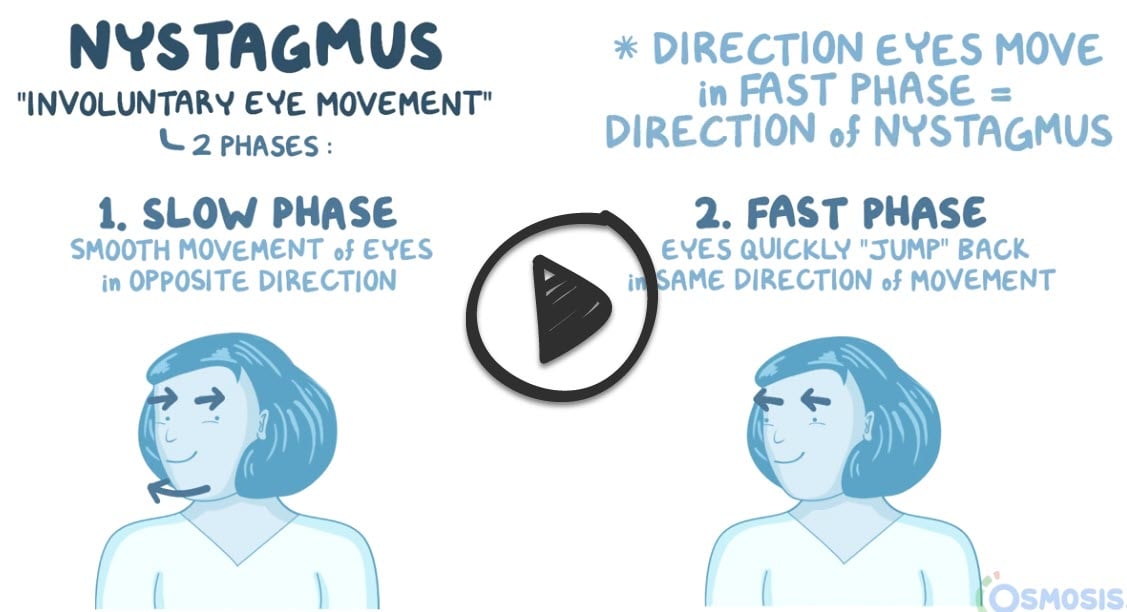
Nystagmus is an involuntary, rapid, and repetitive movement of the eyes
Usually, the movement is side-to-side (horizontal nystagmus), but it can also be up and down (vertical nystagmus) or circular (rotary nystagmus). The movement can vary between slow and fast, and it usually involves both eyes
- Down/upbeat: CNS dysfunction
- Vestibular (horizontal): labyrinth or vestibular nerve dysfunction
- Gaze-evoked: most common and often benign
There are two types of nystagmus: congenital and acquired
1. Congenital nystagmus develops in infancy, usually between six weeks and three months of age. Sensory nystagmus also occurs early in life and is related to poor vision caused by a variety of eye conditions, including cataracts (cloudiness of the eye's lens), strabismus (eye misalignment), and optic nerve hypoplasia. As they get older, children with nystagmus don't see the world as shaky, but they will probably develop less clear vision.
2. Acquired nystagmus occurs later in life and has a variety of causes, including an association with serious medical conditions. Unlike children with nystagmus, adults who acquire nystagmus may see images as shaky.
Caloric reflex test in which one ear canal is irrigated with warm or cold water or air. The temperature gradient provokes the stimulation of the horizontal semicircular canal and the consequent nystagmus
- The resulting movement of the eyes may be recorded and quantified by electronystagmography (ENG), a form of electrooculography (an electrical method of measuring eye movements using external electrodes), or a videonystagmograph (VNG), a form of video-oculography (VOG) (a video-based method of measuring eye movements using external small cameras built into head masks) by an audiologist
- Special swinging chairs with electrical controls can be used to induce rotatory nystagmus
Orthoptists may also use an optokinetic drum or electrooculography to assess a patient's eye movements
Magnetic resonance imaging (MRI) may be necessary to evaluate for intracranial lesions
Congenital nystagmus has traditionally been viewed as non-treatable, but medications have been discovered in recent years that show promise in some patients
- Baclofen can effectively stop periodic alternating nystagmus
- Gabapentin improvement in about half the patients who received it to relieve symptoms of nystagmus
- Other drugs found to be effective against nystagmus in some patients include memantine, levetiracetam, 3,4-diaminopyridine, 4-aminopyridine, and acetazolamide
- Contact lenses and low-vision rehabilitation have also been proposed
- Tenotomy is now being performed regularly at numerous centers around the world
- Acupuncture has conflicting evidence as to having beneficial effects on the symptoms of nystagmus
- Physical therapy or occupational therapy is also used to treat nystagmus. Treatment consists of learning compensatory strategies to take over for the impaired system
- Surgery may be required depending on the cause
Question 1 |
central nervous system (CNS) lesion Hint: Central lesions often have dissociation of the vertigo and nystagmus. The nystagmus in this condition is often vertical and without fatigability with repeated testing. | |
positional vertigo | |
Labyrinthitis | |
Meniere disease | |
vestibular neuronitis |
Question 2 |
Korsakoff psychosis | |
Wernicke encephalopathy | |
acute dystonia | |
acute cocaine toxicity | |
trigeminal neuralgia |
|
List |
References: Merck Manual · UpToDate


 Osmosis
Osmosis