Patient with retinal artery occlusion will present as → a 74-year-old man with sudden vision loss in his right eye. He has a medical history of hypertension, coronary artery disease, and new-onset atrial fibrillation. On physical exam, a carotid bruit is auscultated. His visual acuity is light perception. Confrontational visual fields reveal a dense scotoma, and a penlight examination shows an afferent pupillary defect. Dilated funduscopic examination shows retinal whitening with a cherry-red spot in the fovea.
Patient with retinal vein occlusion will present as → a 65-year-old woman who presents to the ED with the sudden onset of painless vision loss in her left eye. Her past medical history includes hypertension and hyperlipidemia. The patient’s temperature is 98°F (36.7°C), blood pressure is 145/86 mmHg, pulse is 62/min, and respirations are 12/min with an oxygen saturation of 98% O2 on room air. An ophthalmology consult is called, and the fundoscopic examination reveals a swollen optic disc with extensive retinal hemorrhages.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
A retinal artery or vein occlusion, also known as an eye stroke, is a blockage of one of the blood vessels feeding the retina, which is the light-sensitive nerve tissue lining the back of the eye. Both cause a monocular painless vision loss.
- A blockage results in a lack of oxygen getting to the nerve cells in the retina, which may result in drastic vision loss
- Blockages happen in the arteries supplying blood to the retina and veins that take blood away from the eye. These blockages involve most of the retina (central) or a portion of the retina (branch)
- Central retinal artery occlusion (CRAO): This blockage of the main artery supplying blood (and oxygen) to the eye has the highest potential to cause the most damage to the eye, resulting in severe vision loss.
- Branch retinal artery occlusion (BRAO): This is a blockage of one artery in the retina more in the retinal periphery. It causes severe loss of vision in that location but doesn’t typically affect the central vision.
- Central retinal vein occlusion (CRVO): This is a blockage of the main vein that drains blood from the retina and causes severe loss of vision as fresh oxygenated blood cannot get into the eye. This is more common than a CRAO and is associated with high blood pressure and diabetes
- Branch retinal vein occlusion (BRVO): Blockages of the branches of the retinal vein are called branch retinal vein occlusions. These blockages cause blood and fluid to spill into the retina and cause swelling that impacts your ability to see.
-
- Retinal artery occlusion
- Retinal vein occlusion
- Optic neuritis
- Temporal (giant) cell arteritis
Central retinal artery occlusion is characterized by sudden, painless acute visual loss usually attributed to ischemia or thrombus to the major retinal arterial blood supply
- Caused by an embolism resulting from atrial fibrillation, cardiac vegetation, or a patent foramen ovale, but might be also due to thrombosis of the retinal artery, usually as a result of atherosclerosis
- Commonly results from ruptured plaque from the same-sided (ipsilateral) carotid artery
- Typically, the patient presents with sudden, painless onset of markedly decreased unilateral loss of vision (amaurosis fugax)
- Physical examination findings include a significant decrease in visual acuity, relative afferent pupillary defect (ie, Marcus Gunn pupil)
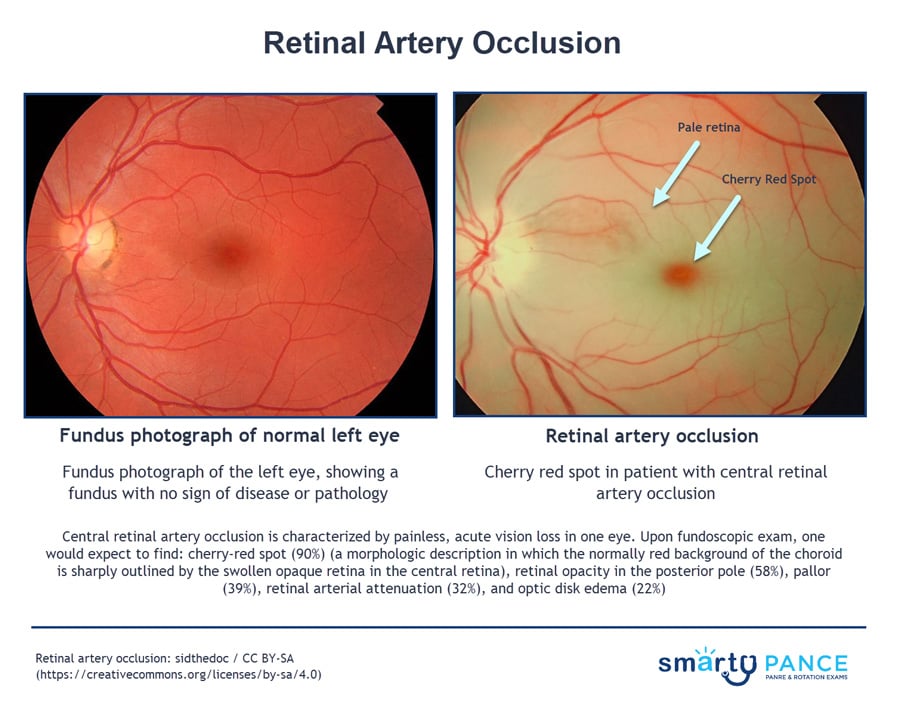
- Fundoscopy reveals a cloudy, pale retina with attenuated vessels and a cherry-red spot in the fovea
- The cherry-red spot is seen because the macula receives its blood supply from the choroid, which remains unaffected, while the surrounding retina is pale and ischemic due to the retinal artery occlusion
Retinal vein occlusion
- This manifests as a sudden acute monocular vision loss
- Can be further divided into non-ischemic and ischemic subtypes
- Compression of the central retinal vein or one of its branches due to a thrombus, a narrow vein, or from an atherosclerotic artery crossing it
- For diagnosis, look for a history of cardiovascular risk factors, such as diabetes mellitus and hypertension, or hypercoagulable states like polycythemia vera
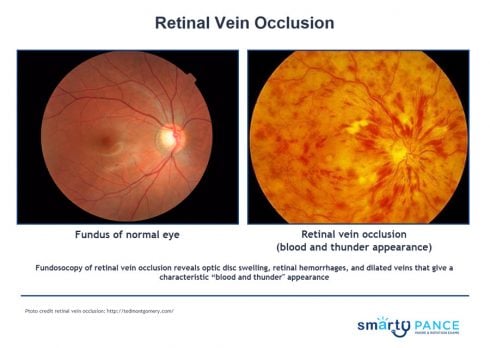
- A fundoscopic examination may reveal optic disc swelling, retinal hemorrhages, and dilated veins that give a characteristic “blood and thunder appearance”
Fundoscopy of retinal artery occlusion ⇒ cherry-red spot on the macula and pale retina
Fundoscopy of retinal vein occlusion ⇒ optic disc swelling, retinal hemorrhages, and dilated veins that give a characteristic “blood and thunder appearance”
Central retinal artery occlusion is an ophthalmologic emergency ⇒ immediate treatment is indicated if occlusion occurred within 24 h of presentation
- Reduction of intraocular pressure with ocular hypotensive drugs (eg, topical timolol 0.5%, acetazolamide 500 mg IV or PO)
- Intermittent digital massage over the closed eyelid or anterior chamber paracentesis may dislodge an embolus and allow it to enter a smaller branch of the artery, thus reducing the area of retinal ischemia
- If patients present within the first few hours of occlusion, some centers catheterize the carotid/ophthalmic artery and selectively inject thrombolytic drugs
- Treatment may include hyperbaric oxygen therapy, which involves the inhalation of 100% oxygen at a pressure that’s higher than the atmospheric pressure
Retinal vein occlusion is treated with laser photocoagulation and steroid or anti-VEGF injections
 Central retinal artery occlusion (CRAO) can cause ischemia to the retina’s sensitive tissue, resulting in vision loss that can be permanent. Etiologies for CRAO are mostly based in thromboembolic phenomena from diseases such as atherosclerosis, atrial fibrillation, and giant cell (temporal) arteritis. Sudden, painless monocular vision loss or a “descending curtain” view are classic symptoms described by patients. There may be retinal plaques on fundoscopy, a grayish discoloration to the retina, or a cherry-red spot on the macula. Ultrasound is helpful in diagnosis. Management includes immediate ocular massage and lowering of intraocular pressure to prevent permanent damage.
Central retinal artery occlusion (CRAO) can cause ischemia to the retina’s sensitive tissue, resulting in vision loss that can be permanent. Etiologies for CRAO are mostly based in thromboembolic phenomena from diseases such as atherosclerosis, atrial fibrillation, and giant cell (temporal) arteritis. Sudden, painless monocular vision loss or a “descending curtain” view are classic symptoms described by patients. There may be retinal plaques on fundoscopy, a grayish discoloration to the retina, or a cherry-red spot on the macula. Ultrasound is helpful in diagnosis. Management includes immediate ocular massage and lowering of intraocular pressure to prevent permanent damage.
| Central retinal artery occlusion (CRAO) | Play Video + Quiz |
| Central retinal vein occlusion | Play Video + Quiz |
Question 1 |
Central retinal artery occlusion Hint: Presents with a cherry-red spot at the macula and retinal whitening. | |
Central retinal vein occlusion | |
Diabetic retinopathy Hint: Typically presents with microvascular changes over time. | |
Hypertensive retinopathy Hint: May have some similar findings but lacks the venous engorgement characteristic of CRVO. | |
Anterior ischemic optic neuropathy Hint: Causes optic disc swelling but lacks the retinal hemorrhages and venous engorgement. |
Question 2 |
Central retinal artery occlusion | |
Central retinal vein occlusion Hint: Central retinal vein occlusion (CRVO) is characterized by painless, unilateral vision loss of varying severity, slower onset of decreased vision than with arterial occlusion, retinal hemorrhages, cotton wool spots, and macular edema. | |
Diabetic retinopathy Hint: Typically causes gradual vision loss with different fundoscopic findings. | |
Hypertensive retinopathy Hint: Presents with findings like arteriolar narrowing and cotton wool spots. | |
Retinal detachment Hint: Usually includes symptoms like flashes and floaters. |
Question 3 |
Presence of cotton wool spots and flame hemorrhages Hint: These findings are more indicative of retinal vein occlusion, which is characterized by venous congestion and hemorrhagic events in the retina. | |
Cherry-red spot at the fovea Hint: While a cherry-red spot is a feature of retinal artery occlusion, it is not typically seen in isolation without retinal whitening. | |
Neovascularization on the retina and optic disc Hint: Neovascularization can be a late complication of retinal vein occlusion due to ischemia-induced proliferation of new blood vessels. | |
Retinal whitening with a cherry-red spot | |
Optic disc swelling and macular edema Hint: These findings can be seen in retinal vein occlusion due to increased venous pressure leading to leakage and swelling. |
Question 4 |
Ophthalmoscopy Hint: While useful for examining the retina, ophthalmoscopy may not reveal any abnormalities in amaurosis fugax, especially outside an acute episode. | |
Schiotz tonometry Hint: This test measures intraocular pressure and is more relevant in the context of glaucoma, not amaurosis fugax. | |
Magnetic Resonance Angiography (MRA) Hint: While MRA can provide detailed images of blood vessels, it is not typically the first-line diagnostic tool for amaurosis fugax. Carotid ultrasound is less invasive and more focused on the common source of emboli. | |
Carotid ultrasound | |
Electroretinography (ERG) Hint: ERG assesses the electrical response of the retina but is not typically used as an initial diagnostic tool for amaurosis fugax. |
Question 5 |
Immediate administration of intravenous tissue plasminogen activator (tPA) | |
High-dose oral prednisone Hint: This is not a standard treatment for CRAO, as corticosteroids do not address the underlying arterial occlusion. | |
Topical beta-blocker eye drops Hint: While beta-blockers can lower intraocular pressure, they are not effective in treating CRAO, as they do not dissolve or dislodge the occluding clot. | |
Hyperbaric oxygen therapy Hint: Although hyperbaric oxygen can increase oxygen delivery to ischemic tissues, its role in the acute management of CRAO is not well established and is not considered a first-line treatment. | |
Conservative management with observation Hint: CRAO is an ophthalmic emergency, and immediate intervention is crucial. Conservative management is not appropriate due to the risk of permanent vision loss. |
Question 6 |
Panretinal photocoagulation Hint: This treatment is used in cases of proliferative diabetic retinopathy and certain cases of CRVO with neovascularization, but it is not the first-line treatment for acute CRVO without neovascular complications. | |
Intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) agents | |
Systemic anticoagulation with warfarin Hint: Anticoagulation is not typically used in the management of CRVO, as the condition involves venous congestion rather than an arterial clot. | |
Topical beta-blocker eye drops Hint: These are used to lower intraocular pressure in conditions like glaucoma but do not address the underlying pathology of CRVO. | |
Immediate administration of intravenous tissue plasminogen activator (tPA) Hint: tPA is used in arterial occlusions, such as central retinal artery occlusion, but not in venous occlusions like CRVO. |
Question 7 |
Immediate laser photocoagulation Hint: Used in certain cases of retinal vein occlusion with neovascularization. | |
Intravitreal injection of anti-VEGF agents Hint: Indicated for macular edema secondary to vein occlusion. | |
Systemic anticoagulation Hint: Typically not used in central retinal vein occlusion unless there is a specific indication like a coexisting systemic thromboembolic disorder. | |
Observation and control of systemic risk factors | |
Surgical embolectomy Hint: Not a standard treatment for retinal vein occlusion. |
|
List |
References: Merck Manual (artery) (vein)· UpToDate (artery) (vein)


 Lecture
Lecture Picmonic
Picmonic