Patient with diabetic retinopathy will present as → a 65-year-old woman with a 10-year history of type 2 diabetes mellitus presents for a routine eye examination. She reports no visual symptoms. Her last eye examination was 2 years ago. On fundoscopic examination, you note microaneurysms, dot and blot hemorrhages, and hard exudates in both eyes. There is no evidence of neovascularization or vitreous hemorrhage.
Patient with hypertensive retinopathy will present as → a 64-year-old undergoing an ocular exam during a routine medical check-up. PMH is remarkable for essential hypertension. The patient's BP is 160/90, and he has been nonadherent to his antihypertensive regimen. Retinal examination demonstrates generalized retinal arteriolar narrowing, arteriovenous (AV) nicking, broad and dull light reflex, flame-shaped hemorrhages in two areas, and multiple cotton wool spots.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Retinopathy occurs when blood vessels in the back of the eye, the retina, become damaged
- The main causes of retinopathy are hypertensive retinopathy and diabetic retinopathy
- Diabetic retinopathy is the most common cause of new, permanent vision loss and/or blindness in 25-74-year-olds
Diabetic retinopathy ⇒ damage to retinal blood vessels leads to retinal ischemia and edema. Excess sugar attaching to proteins such as the collagen of blood vessels (glycosylation) causes capillary wall breakdown
- Usually asymptomatic until late stages when it causes painless visual impairment that can progress to blindness
- Diabetic retinopathy falls into two main classes: nonproliferative (early) and proliferative (late, advanced)
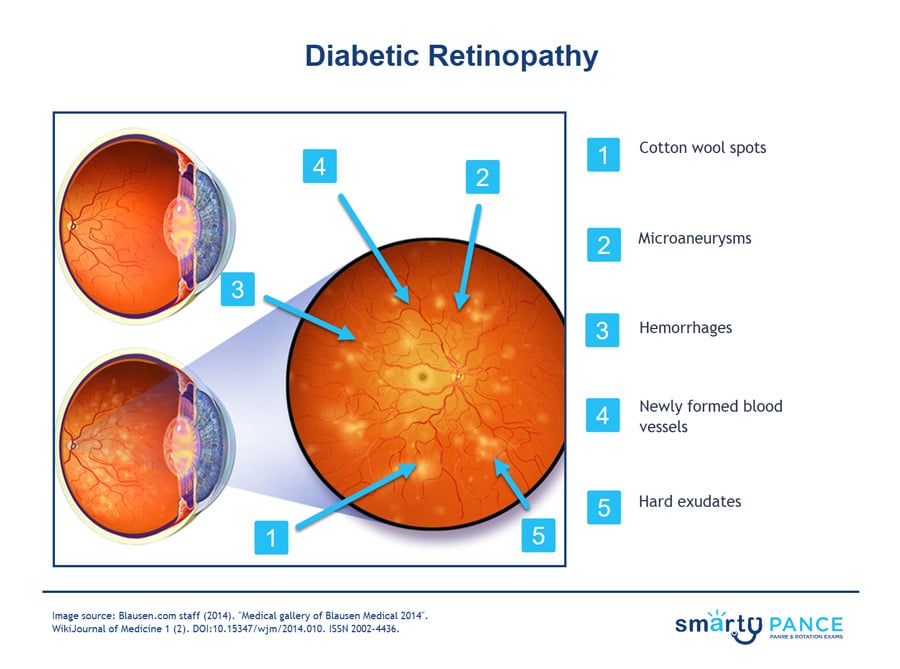
- Nonproliferative ⇒ microaneurysms (visible as red dots), cotton wool spots (fluffy white patches on the retina), hemorrhages, and hard exudates
- Proliferative ⇒ all of the above + neovascularization
Hypertensive retinopathy ⇒ results from retinal arteriolar spasm and narrowing in response to longstanding hypertension
- Often asymptomatic until the late stages may present with decreased or blurred vision
- Silver wiring and AV nicking are the characteristic findings on retinal examination. Retinal hemorrhages suggest an associated retinal vascular accident
- Cotton wool spots, flame hemorrhages, and disc swelling are more typical of malignant hypertension, especially in young patients
Other types of retinopathy are divided by cause – Inflammatory or Infectious
- Inflammatory: Bechet's, Sarcoidosis, SLE, Giant cell arteritis, Polyarteritis nodosa
- Infectious: Syphilis, Herpes simplex, Varicella-Zoster, Toxoplasmosis, and CMV = HIV
Diagnosis is by funduscopy
Diabetic retinopathy
- Nonproliferative type (an early form of the disease)
- Non-proliferative diabetic retinopathy (NPDR) is the early stage of the disease in which symptoms will be mild or nonexistent
- In NPDR, the blood vessels in the retina are weakened
- Fundoscopy: Microaneurysms, hard exudates, cotton wool spots, blot and dot hemorrhages, and venous dilation
- Proliferative type (most severe, abnormal blood vessel growth)
- Proliferative diabetic retinopathy (PDR) is the more advanced form of the disease
- At this stage, circulation problems deprive the retina of oxygen. As a result, new, fragile blood vessels can begin to grow in the retina and into the vitreous. The new blood vessels may leak blood into the vitreous, clouding vision
- Fundoscopic exam (abnormal growth of vessels) neovascularization
Hypertensive retinopathy
- Microaneurysms and cotton-wool spots (also seen in nonproliferative diabetic retinopathy)
- Macular star results from the star-like deposition of exudates into the macula
- Flame-shaped retinal hemorrhages
- Arteriovenous nicking - seen when an arteriole with a thick arteriosclerotic wall compresses a vein that it happens to cross, so this vein bulges on both sides next to the crossing
- In severe cases, papilledema can also be seen
Diabetic retinopathy
- Treatment of non-proliferative diabetic retinopathy relies on blood glucose control
- Treatment of proliferative diabetic retinopathy can be managed with antivascular endothelial growth factor (anti-VEGF) injections (eg, ranibizumab, bevacizumab), peripheral retinal photocoagulation, or surgery
- Yearly dilated ophthalmoscopic examination
Hypertensive retinopathy
- Control of blood pressure and lipids are the mainstay of treatment for hypertensive retinopathy, with laser treatment as determined by a retinal specialist
 Diabetic retinopathy is caused by damage to the blood vessels in the tissue at the back of the eye (retina). Poorly controlled blood sugar is a risk factor. Early symptoms include floaters, blurriness, dark areas of vision, and difficulty perceiving colors. Blindness can occur. Mild cases may be treated with careful diabetes management. Advanced cases may require laser treatment or surgery
Diabetic retinopathy is caused by damage to the blood vessels in the tissue at the back of the eye (retina). Poorly controlled blood sugar is a risk factor. Early symptoms include floaters, blurriness, dark areas of vision, and difficulty perceiving colors. Blindness can occur. Mild cases may be treated with careful diabetes management. Advanced cases may require laser treatment or surgery
Question 1 |
Hypertension | |
Diabetes mellitus | |
Macular degeneration Hint: See B for explanation. | |
Retinal artery occlusion Hint: See B for explanation. |
Question 2 |
maternal rubella infection Hint: While maternal rubella infection is a risk factor for ocular disease in the newborn, it is not a specific risk for retinopathy of prematurity. | |
maternal alcohol abuse Hint: Maternal alcohol abuse is associated with the development of fetal alcohol syndrome, which includes craniofacial abnormalities, but does not include increased risk for retinopathy of prematurity. | |
perinatal oxygen therapy | |
family history of retinal detachment Hint: If retinopathy of prematurity is not treated, retinal detachment may occur causing blindness. A family history of retinal detachment is not considered a risk factor for the development of retinopathy of prematurity. |
Question 3 |
Panretinal laser photocoagulation | |
Iridectomy Hint: Iridectomy is of no value in preserving the retina and iridectomy is harmful in this situation due to the trauma it causes to the eye. | |
Radial keratotomy Hint: Radial keratotomy is indicated to correct myopia. This surgery destroys normal eye architecture and has no benefit in diabetic retinopathy. | |
Vitrectomy Hint: Vitrectomy is indicated for treatment of retinal tears and not to preserve an intact retina. |
Question 4 |
Drusen Hint: Drusen are tiny to small yellowish round spots with hard or soft edges that are often seen in age-related macular degeneration. | |
Cotton-wool patches | |
Hard exudates Hint: Hard exudates are yellowish bright lesions with well-defined borders. They are often small and round. | |
Preretinal hemorrhages Hint: Preretinal hemorrhages obscure the underlying retinal vessels and are seen as a horizontal line of demarcation with plasma above and cells below. |
Question 5 |
Cytomegalovirus retinitis Hint: See C for explanation. | |
Diabetic retinopathy Hint: See C for explanation. | |
Hypertensive retinopathy | |
Sickle cell retinopathy Hint: See C for explanation. |
Question 6 |
He can wait until next year when he goes to get his refraction Hint: In type 2 diabetes, retinopathy is present in up to 20% of patients at diagnosis and may be the presenting feature. Eye examination for vision usually does not require a dilated eye exam, and refraction is not calculated with ophthalmoscope or direct visualization but by refractometer which does not examine the retina where retinopathy occurs. | |
He does not need to see an ophthalmologist if his Hemoglobin A1C is < 6.0 Hint: See C for explanation. | |
Retinopathy is present in 20% of patient with type 2 Diabetes Mellitus at time of diagnosis | |
Your non-dilated exam can substitute for this referral Hint: See C for the explanation. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture